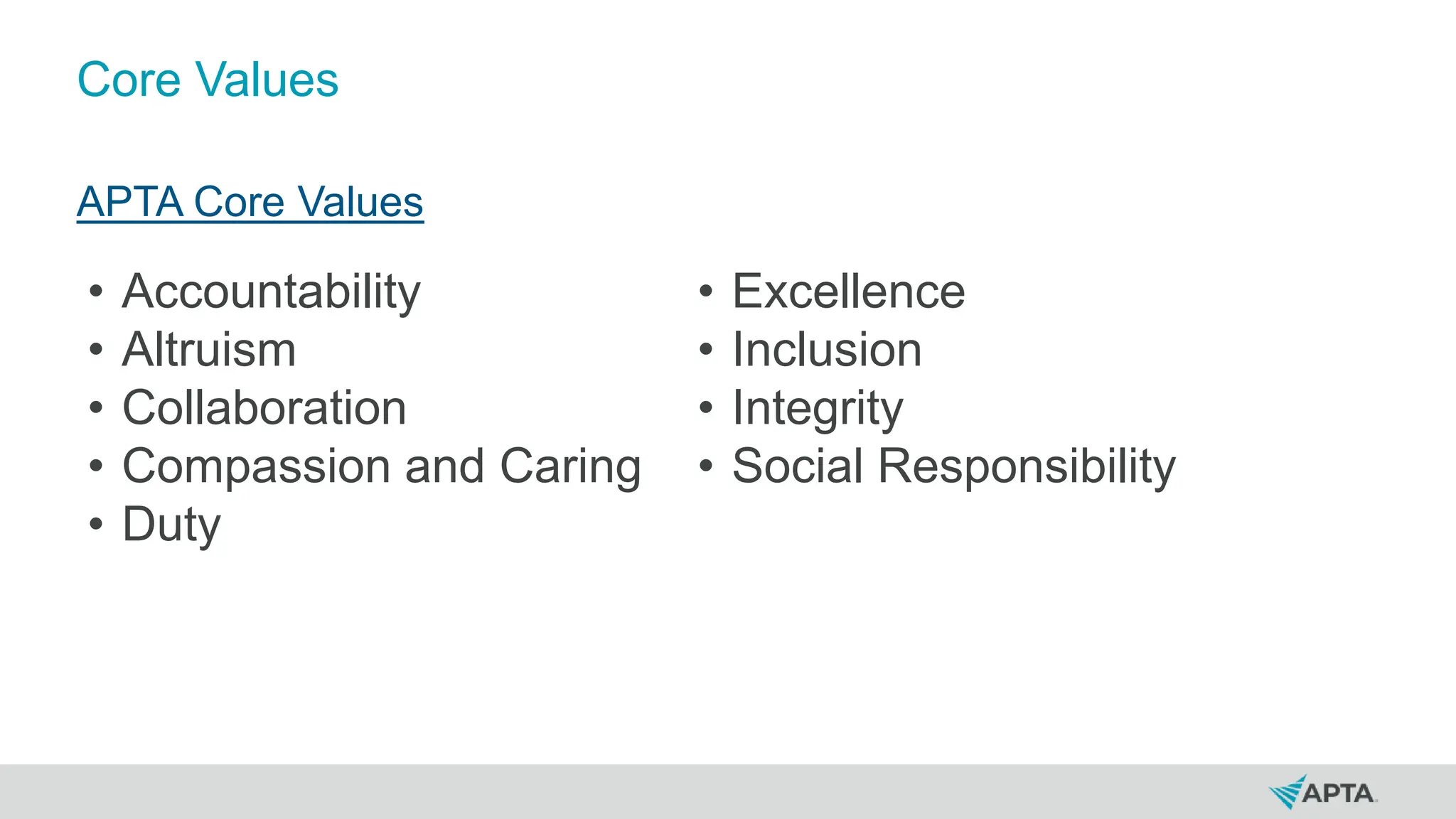
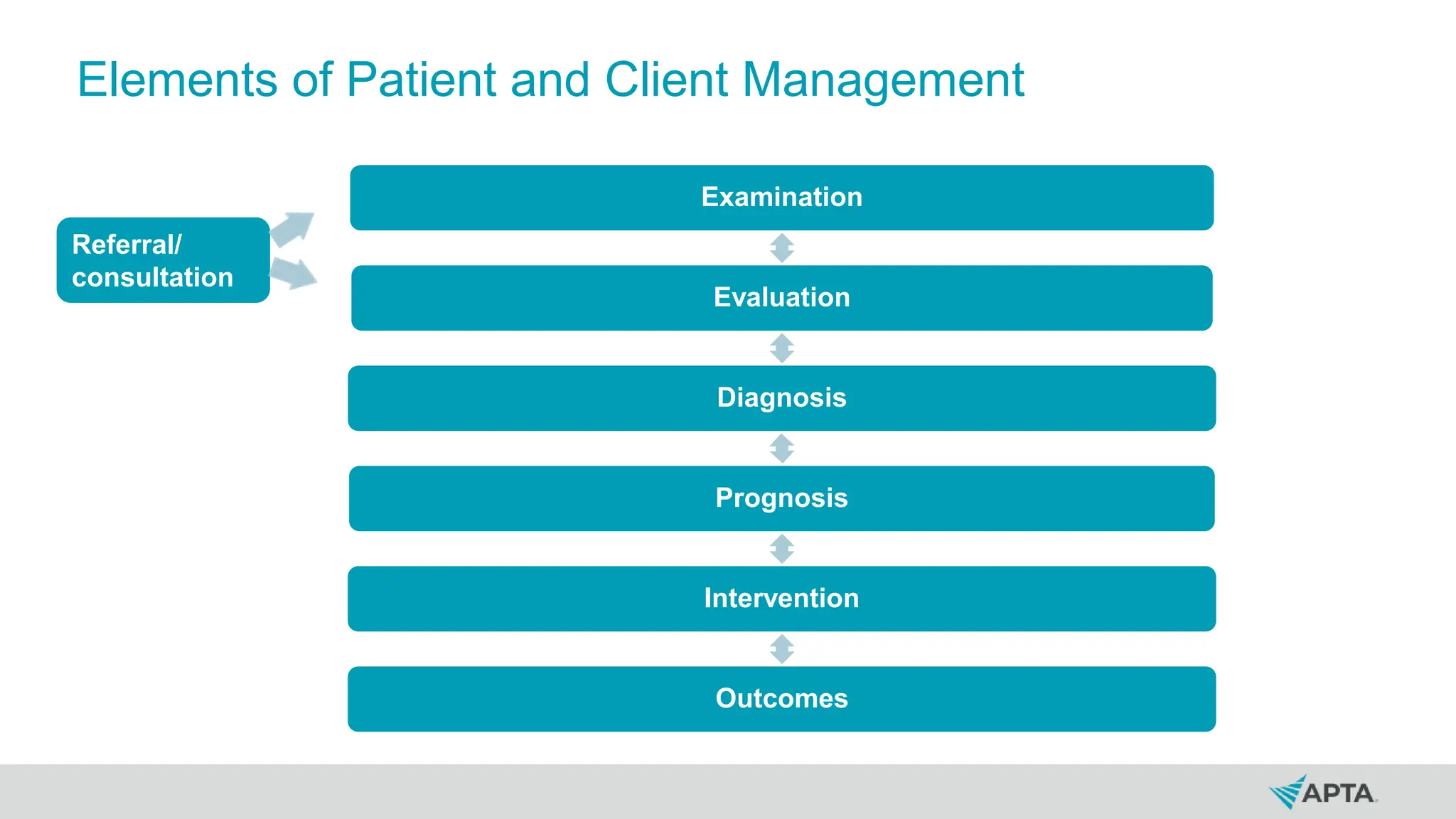
The document provides an overview of the APTA Guide to Physical Therapist Practice, emphasizing the role of physical therapists in diagnosing and managing movement dysfunction to promote optimal health. It outlines core concepts such as evidence-based practice, professional values, and the importance of the biopsychosocial model and social determinants of health in patient care. The document also covers the standards of practice, examination procedures, and the roles of physical therapists and assistants within various healthcare settings.