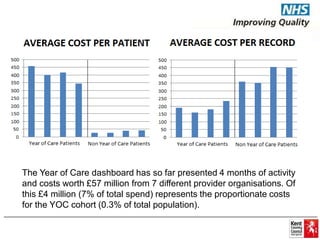
The document discusses the Year of Care (YOC) program in Kent, aimed at improving integrated care by sharing data and information across health services. Key findings and activities highlight the identification and risk stratification of patients with long-term conditions, leading to a shift from service-oriented to patient-focused care planning. It emphasizes the importance of collaboration among various health entities and stakeholders to develop personalized care strategies for individuals with complex health needs.