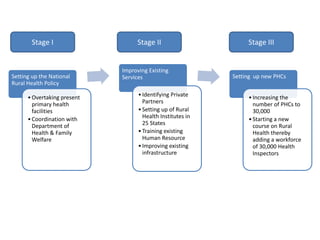
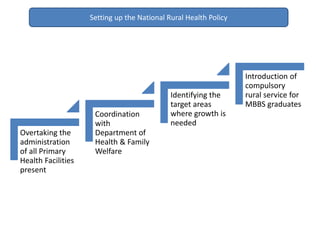
The document discusses a proposed National Rural Health Policy in India to address healthcare issues in rural areas. The key points of the policy are:
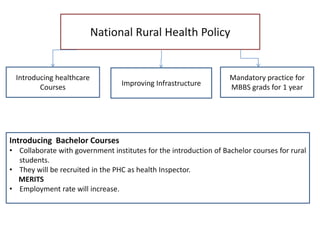
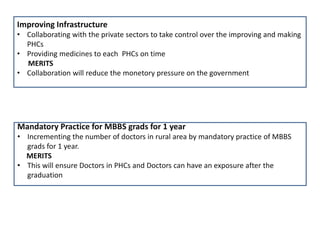
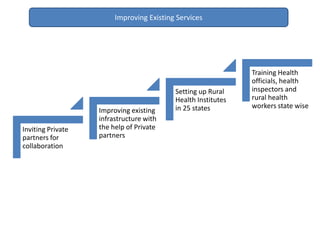
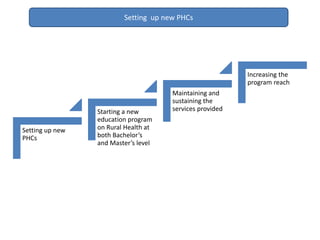
1) Establishing community-government-private partnerships to take over existing primary health facilities and set up new PHCs and rural health institutes.
2) Mandating one year of rural service for MBBS graduates to increase the number of doctors in rural areas.
3) Introducing bachelor's and master's programs in rural health to generate 30,000 new health inspectors and workers.
4) Improving existing infrastructure and services by collaborating with private partners.