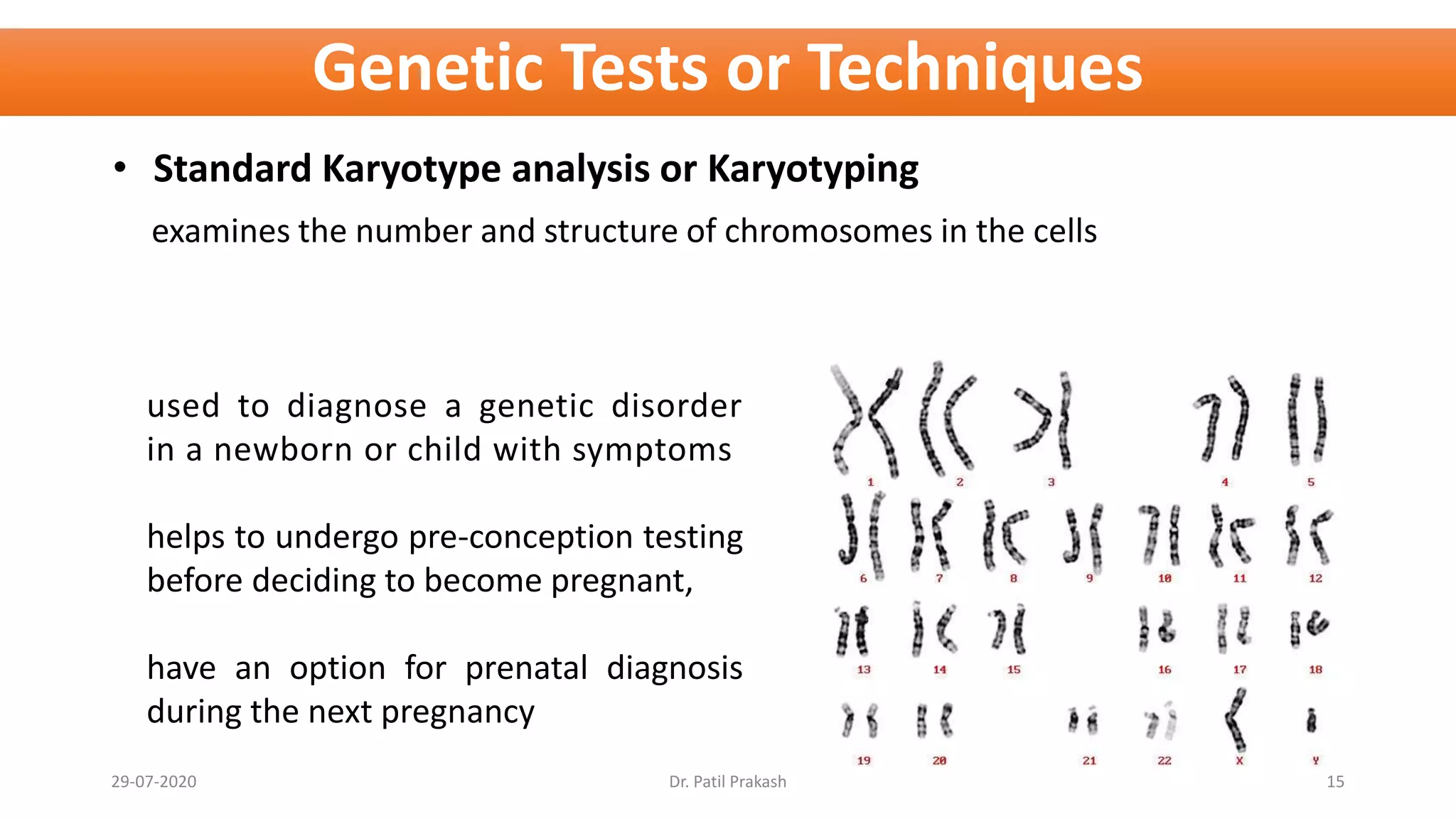
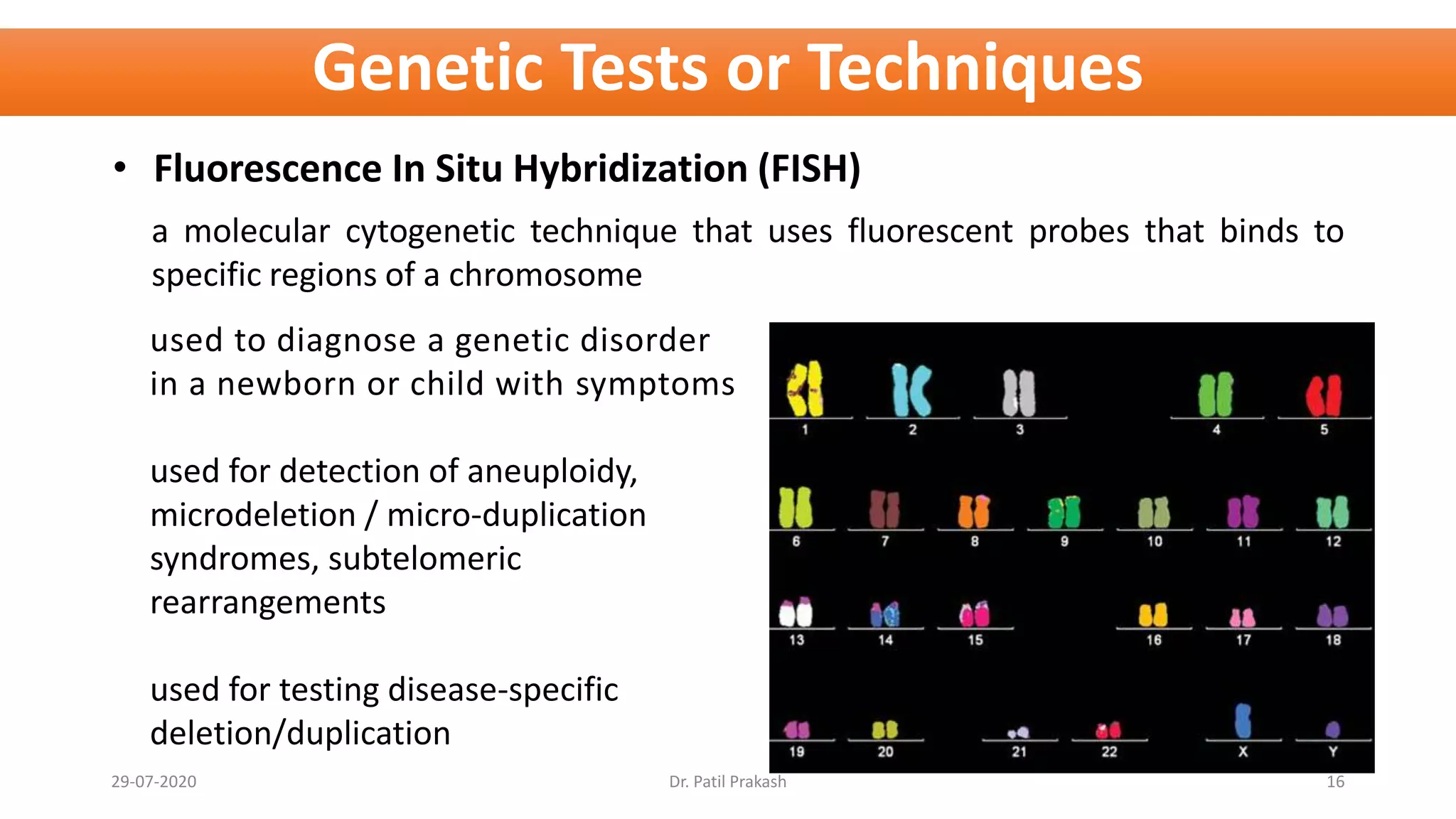
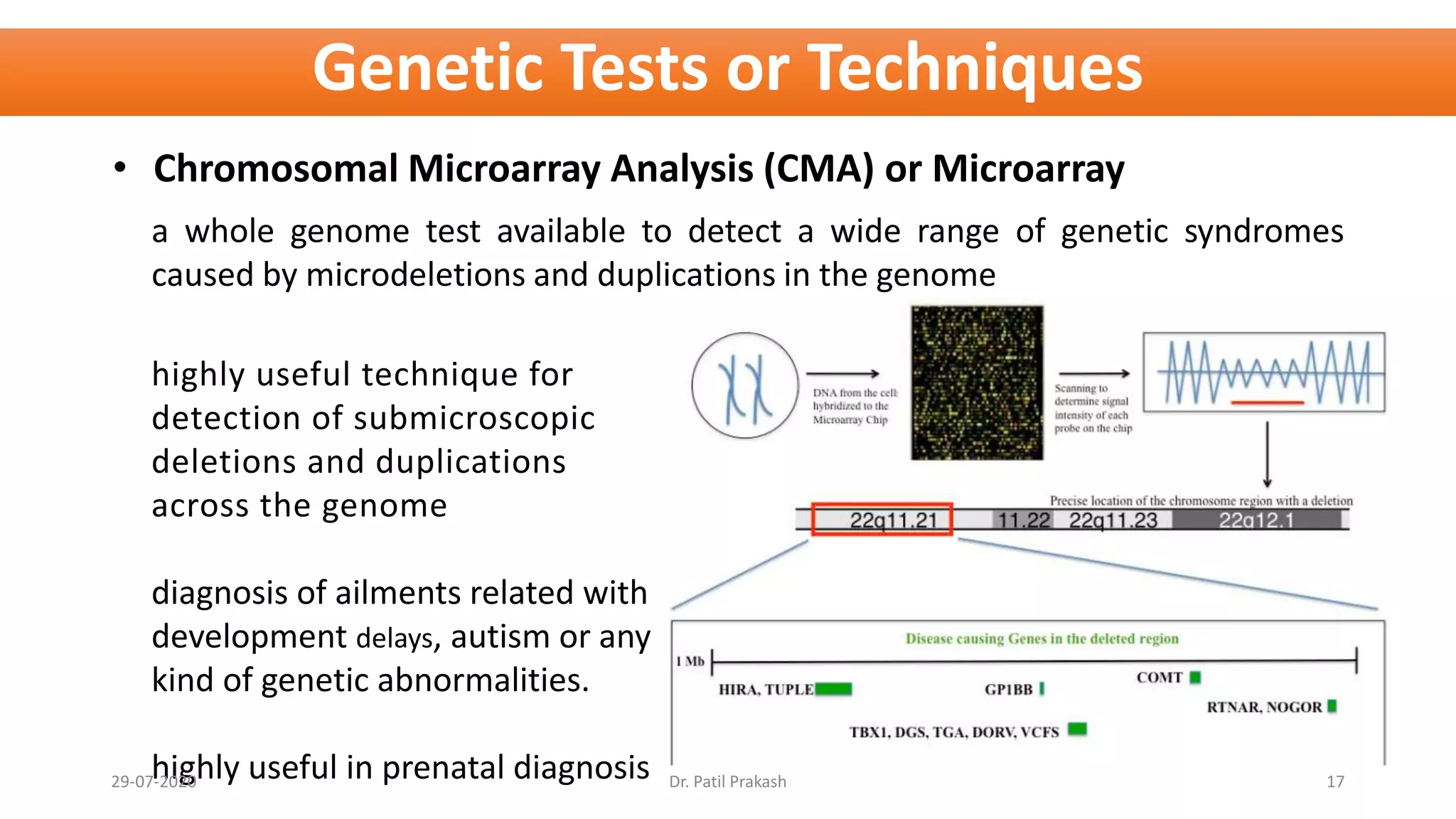
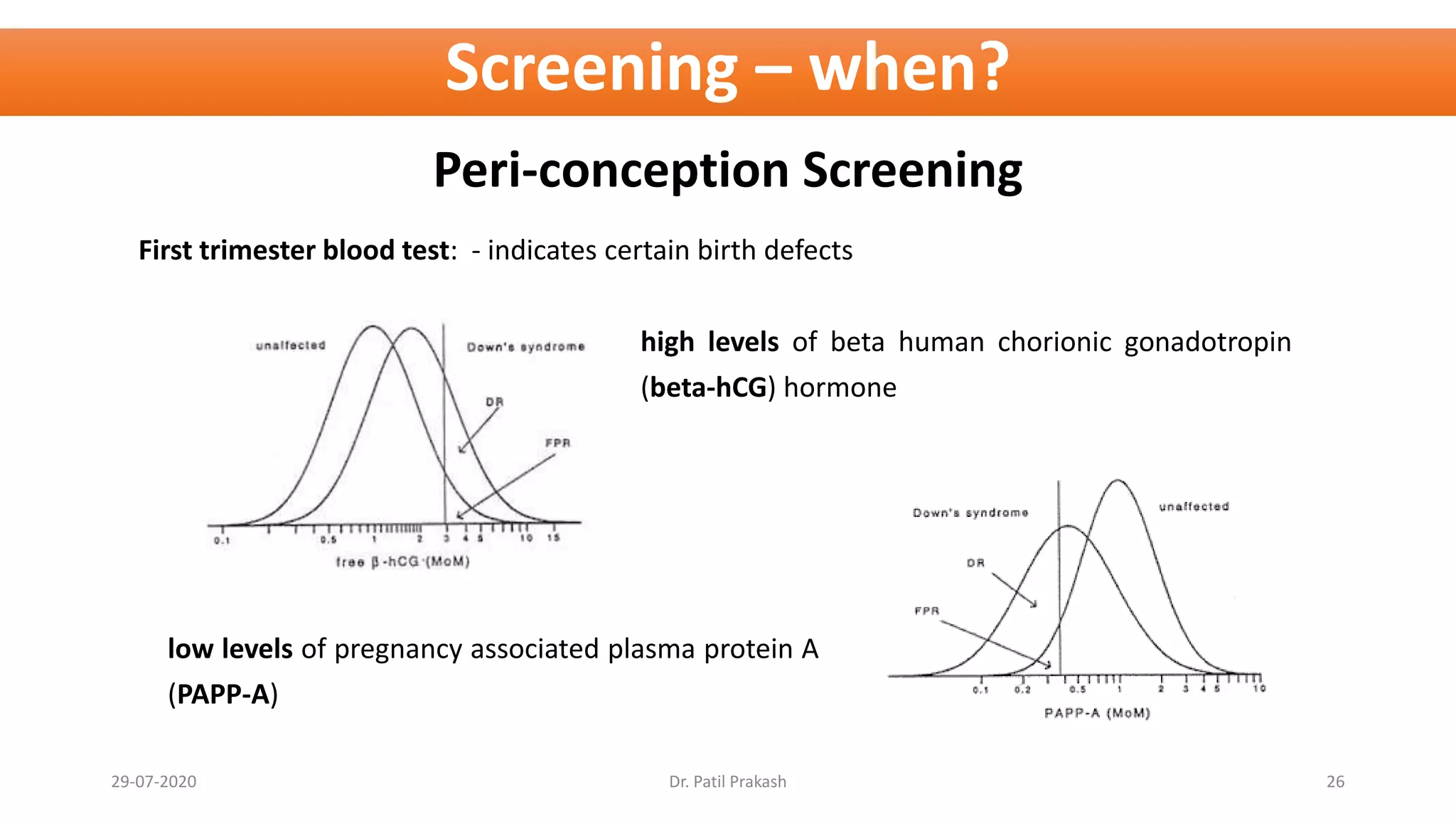
Genetic testing in neonates and children can help diagnose congenital abnormalities. Around 1 in 35 children are born with congenital anomalies that affect development or functioning. Common birth defects in India include congenital heart disease, deafness, and neural tube defects. Genetic testing techniques like karyotyping, fluorescence in situ hybridization (FISH), chromosomal microarray analysis (CMA), and next generation sequencing (NGS) can help identify genetic disorders, chromosomal abnormalities, and mutations that cause congenital anomalies. Genetic testing provides medical benefits through diagnosis but also raises issues regarding psychological impacts, reproductive choice, and potential harms.