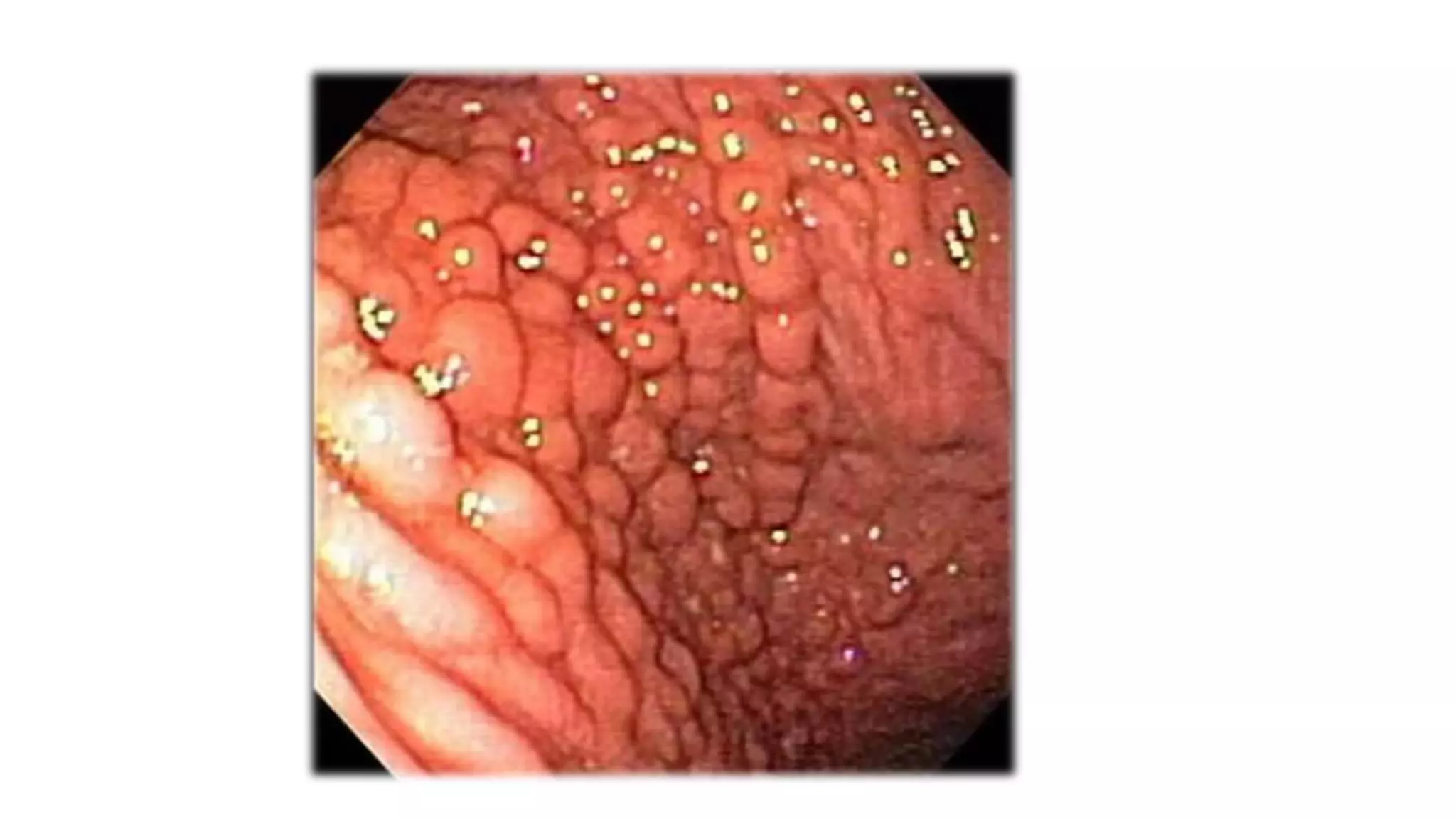
Gastritis is inflammation of the stomach lining that has many potential causes. It can be acute, caused by infections like H. pylori, or chronic. Chronic gastritis is classified as type A, which affects the stomach body and is autoimmune, or type B, which is antral-predominant and usually caused by H. pylori. Treatment involves eradicating the underlying cause, like H. pylori, and treating complications. Rare forms include lymphocytic, eosinophilic, and Menetrier's disease, characterized by large folds in the stomach lining.