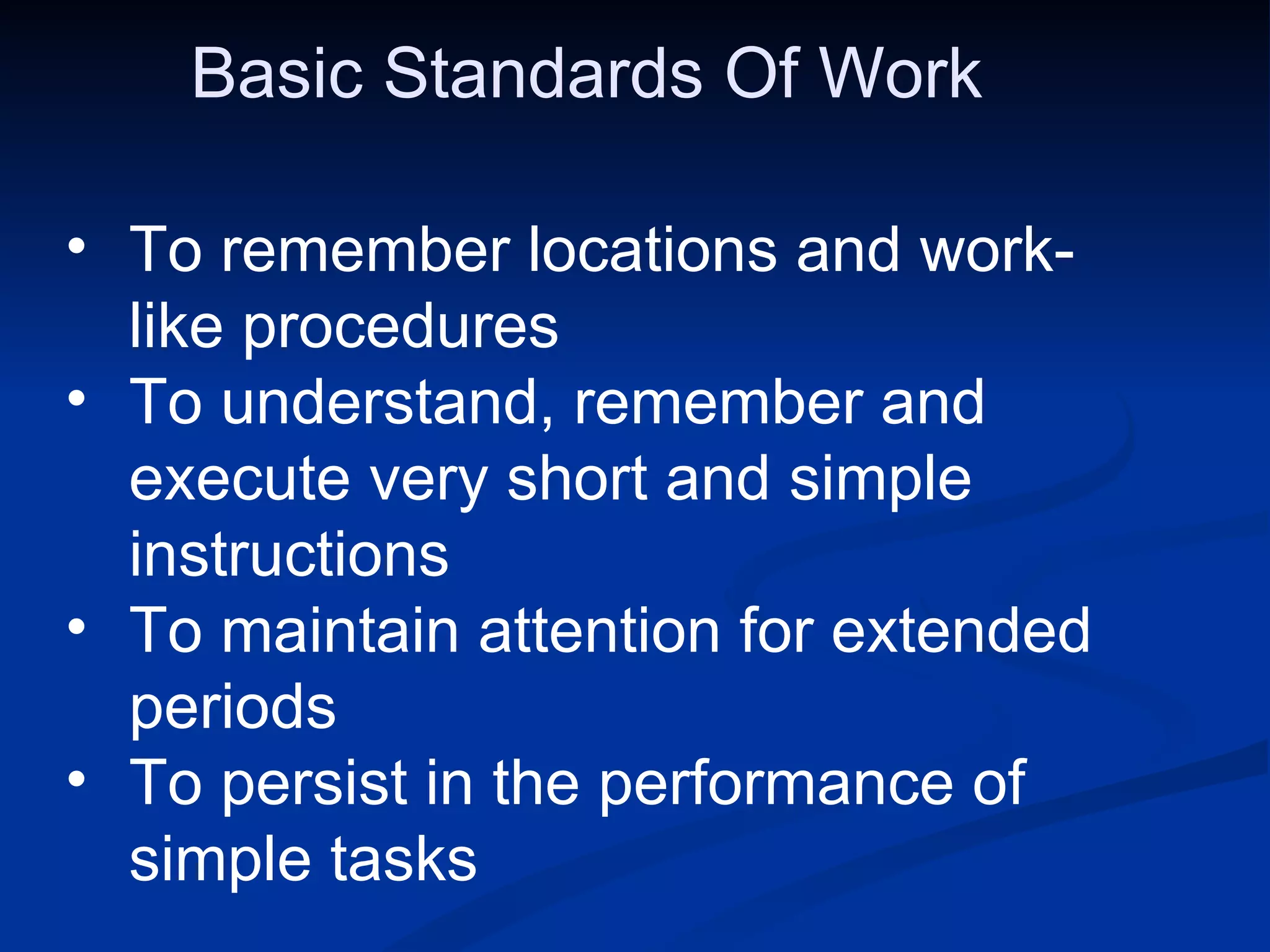
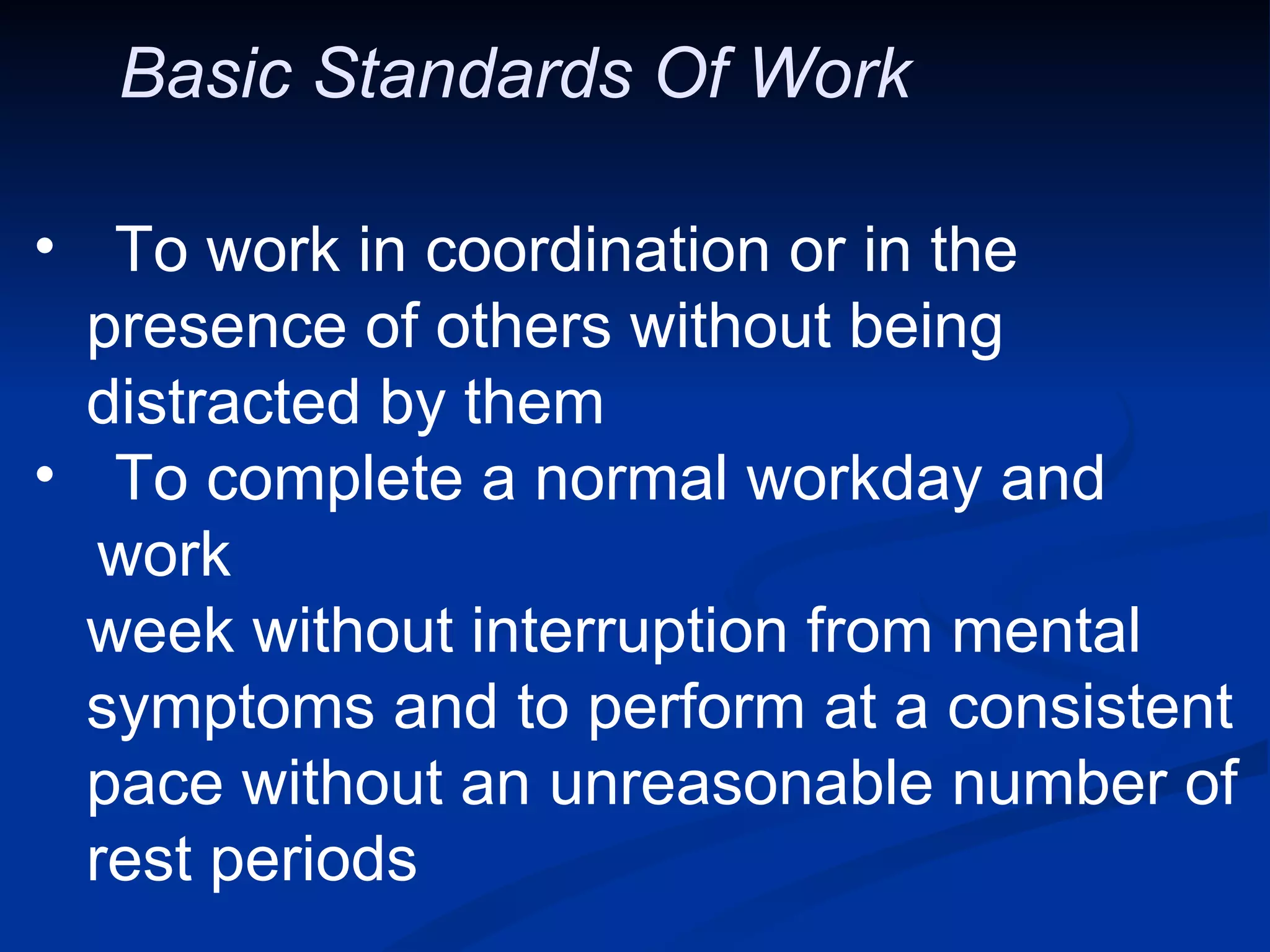
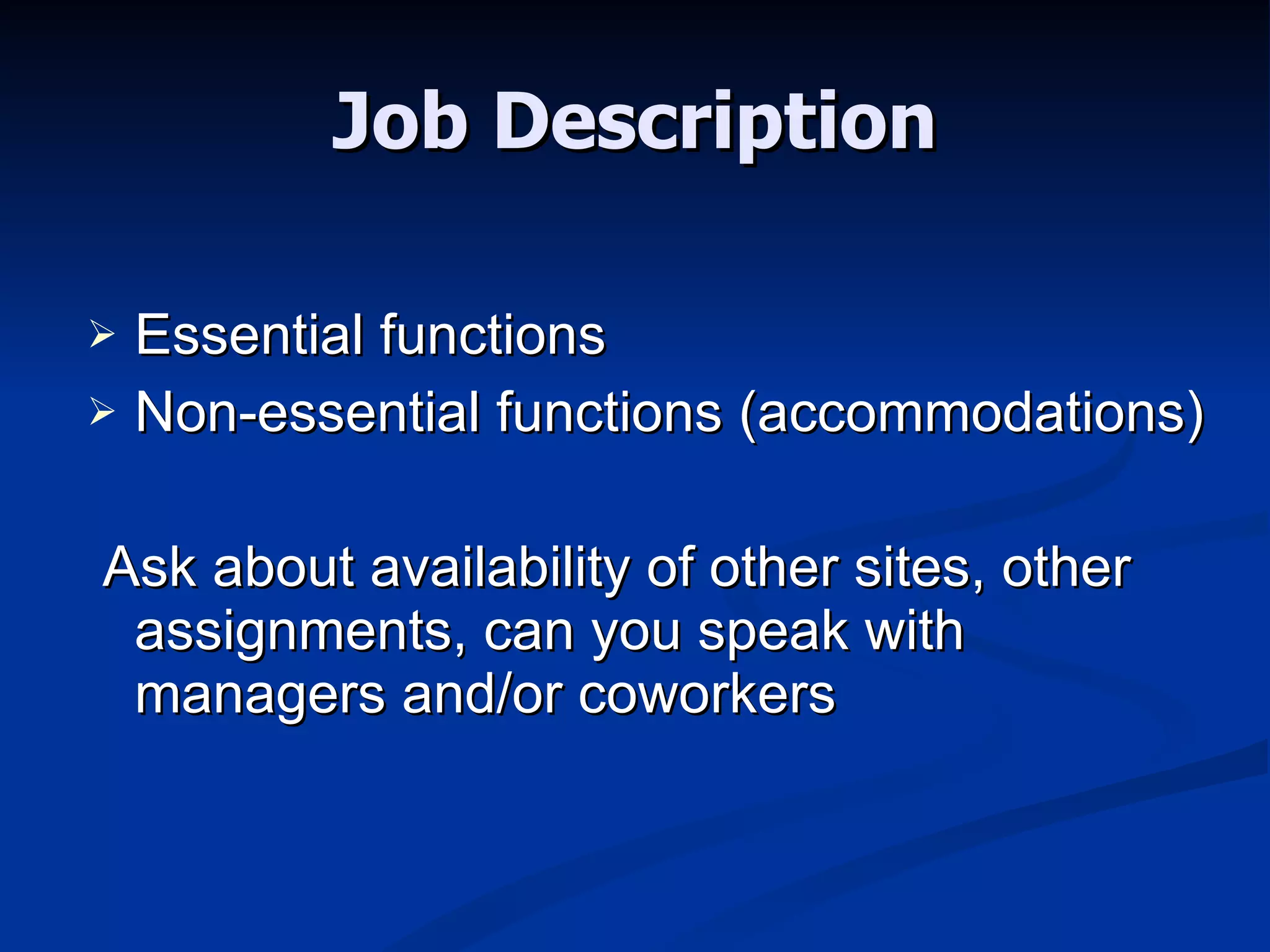
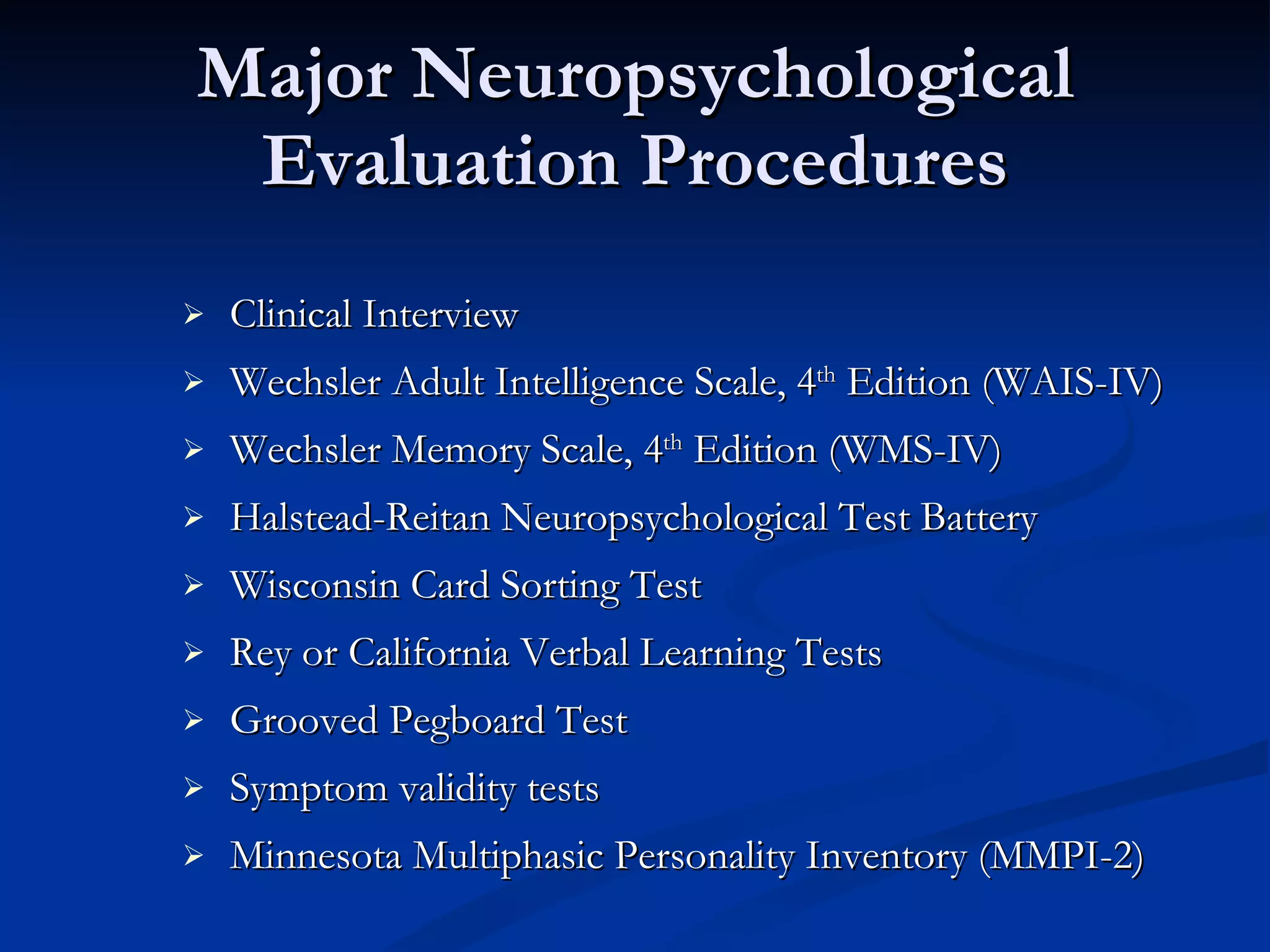
The document discusses fitness-for-duty evaluations, which determine if an employee can safely perform their job duties. It outlines standards of basic work functions and describes tools used in neuropsychological evaluations. Risk factors are assessed like substance abuse, mental health history, and coping skills. The document provides guidance on accommodating disabilities to help employees return to work.























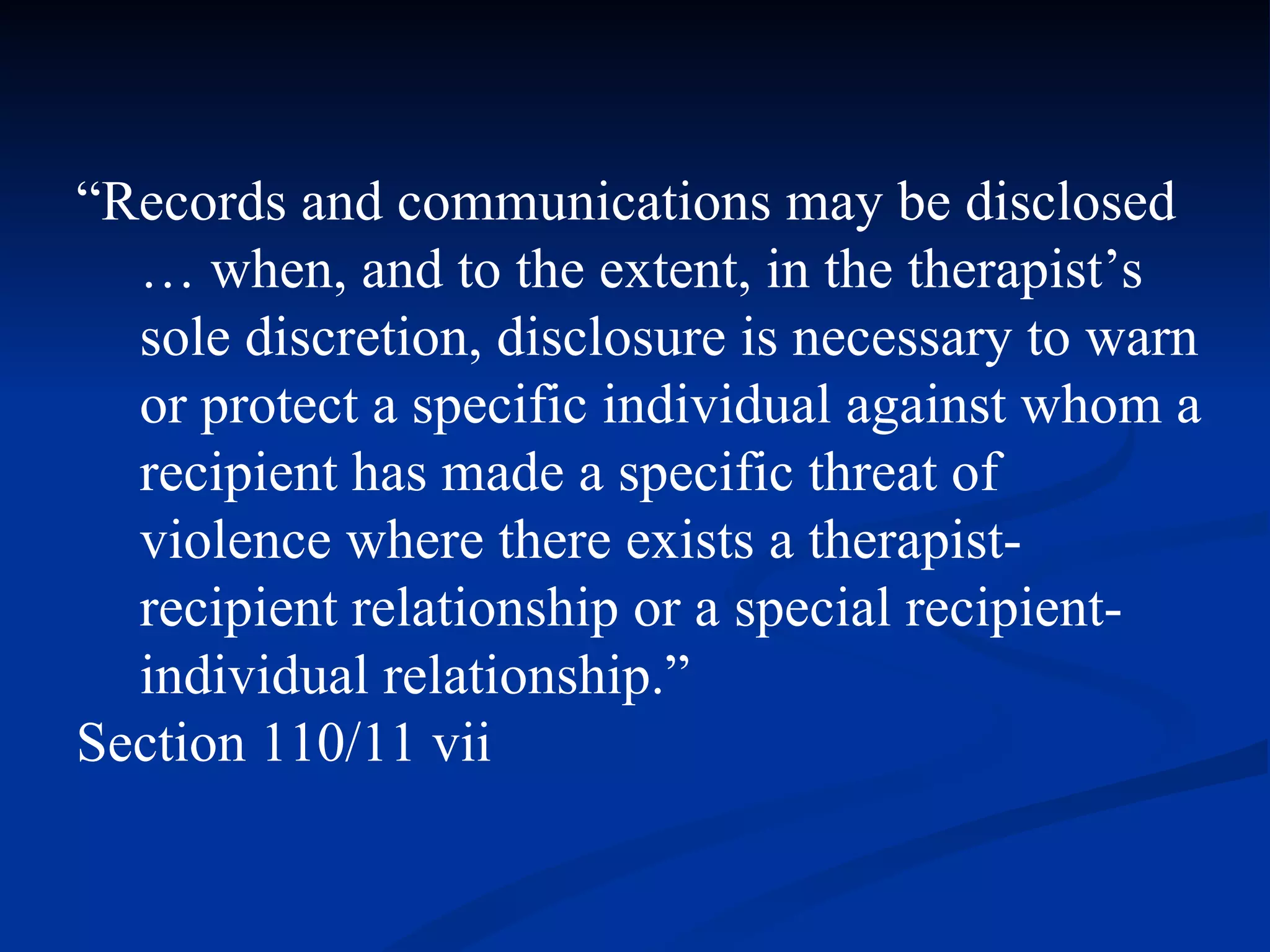
![“ Records and communications may be disclosed … when, and to the extent, a therapist, in his or her sole discretion, determines that such a disclosure is necessary to continue civil commitment proceedings or to otherwise protect the recipient [patient, examinee] or other person against a clear, imminent risk of serious physical or mental injury or disease or death being inflicted upon the recipient, or by the recipient on himself or another.” Section 110/11 ii](https://image.slidesharecdn.com/fitnessfordutyandriskassessments-12590287845643-phpapp02/75/Fitness-For-Duty-And-Risk-Assessments-39-2048.jpg)







![For More Information Steven E. Rothke, Ph.D, ABPP (847) 480-5744 [email_address]](https://image.slidesharecdn.com/fitnessfordutyandriskassessments-12590287845643-phpapp02/75/Fitness-For-Duty-And-Risk-Assessments-54-2048.jpg)