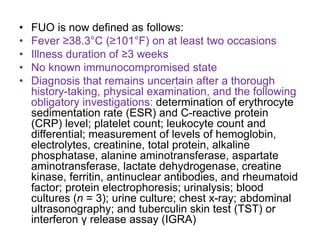
This document discusses fever of unknown origin (FUO), defined as a fever over 101°F for at least 3 weeks without a confirmed diagnosis after initial testing. It outlines the standard tests used to evaluate FUO and describes treatment approaches like antibiotics, anti-tuberculosis drugs, anti-inflammatory drugs, glucocorticoids, and interleukin-1 inhibitors. Imaging with fluorodeoxyglucose positron emission tomography can help guide biopsies. While sometimes challenging to diagnose, FUO often has a favorable prognosis even if the specific cause is never identified.