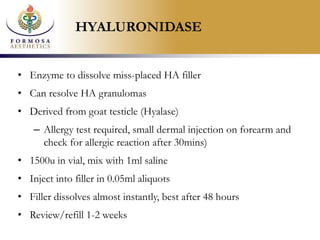
This document discusses complications of dermal fillers, how to avoid them, and their management. It begins by defining filler complications and categorizing them as immediate, early, or late onset. It then discusses various types of complications including technical errors, inflammatory reactions, infections, and immune reactions. The document provides tips for minimizing risks such as obtaining informed consent, using proper technique, understanding anatomy, and following up with clients. It also reviews how to manage specific complications like nodules, granulomas, necrosis, and unhappy clients. The overall goal is to help practitioners understand, avoid, and address any adverse events from dermal fillers.