1. The document discusses respiratory emergencies like acute exacerbations of asthma and COPD.
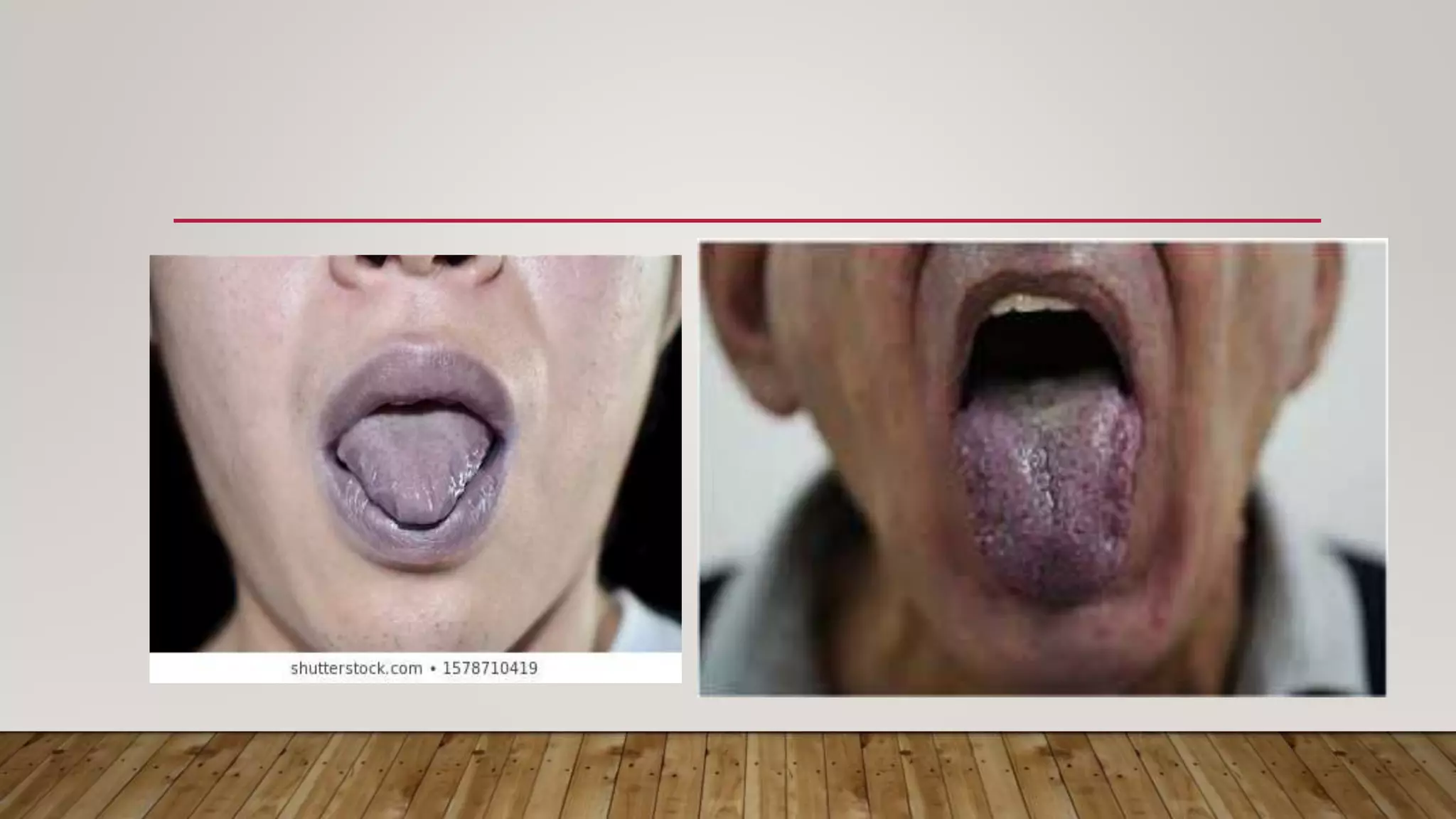
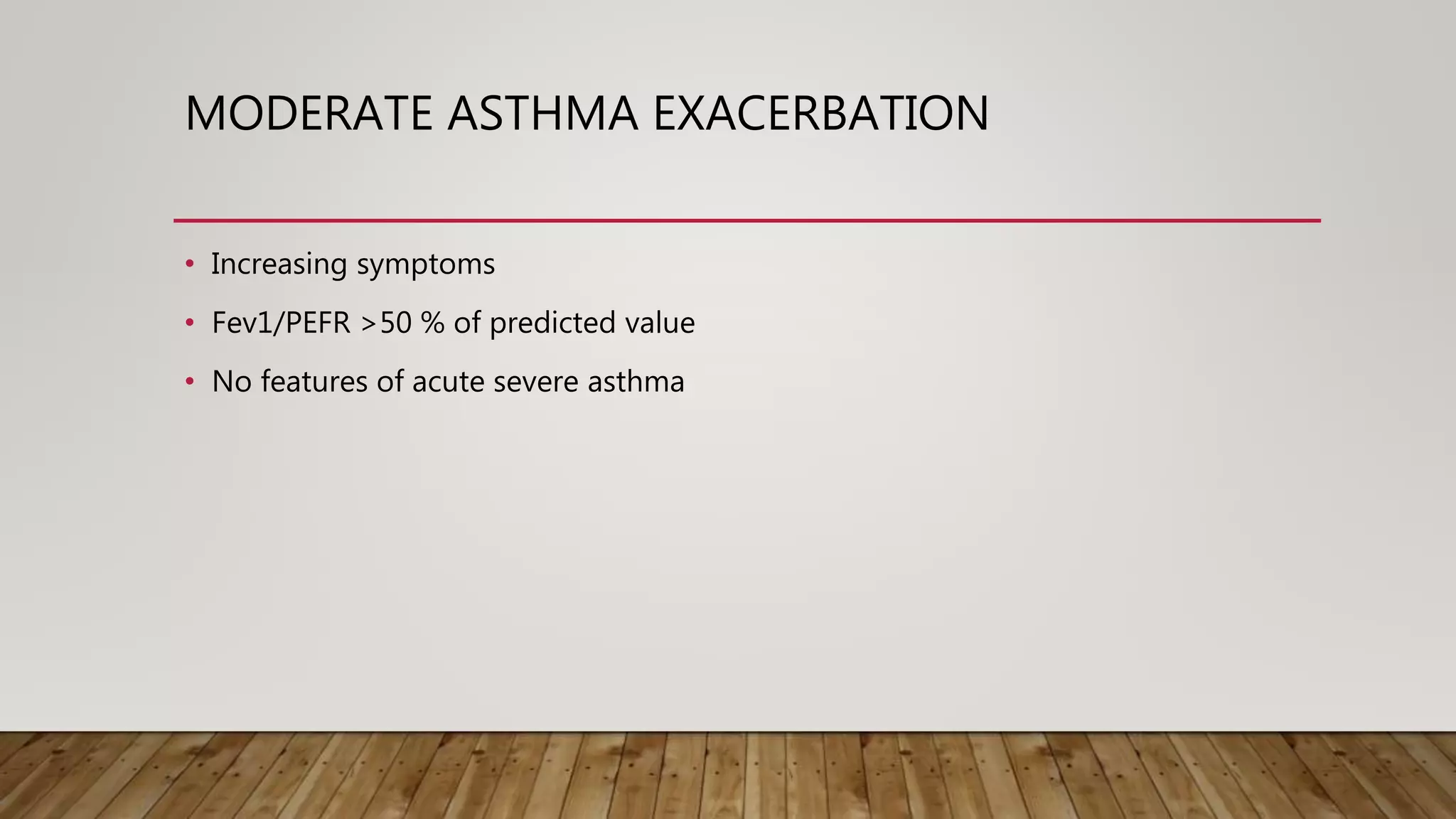
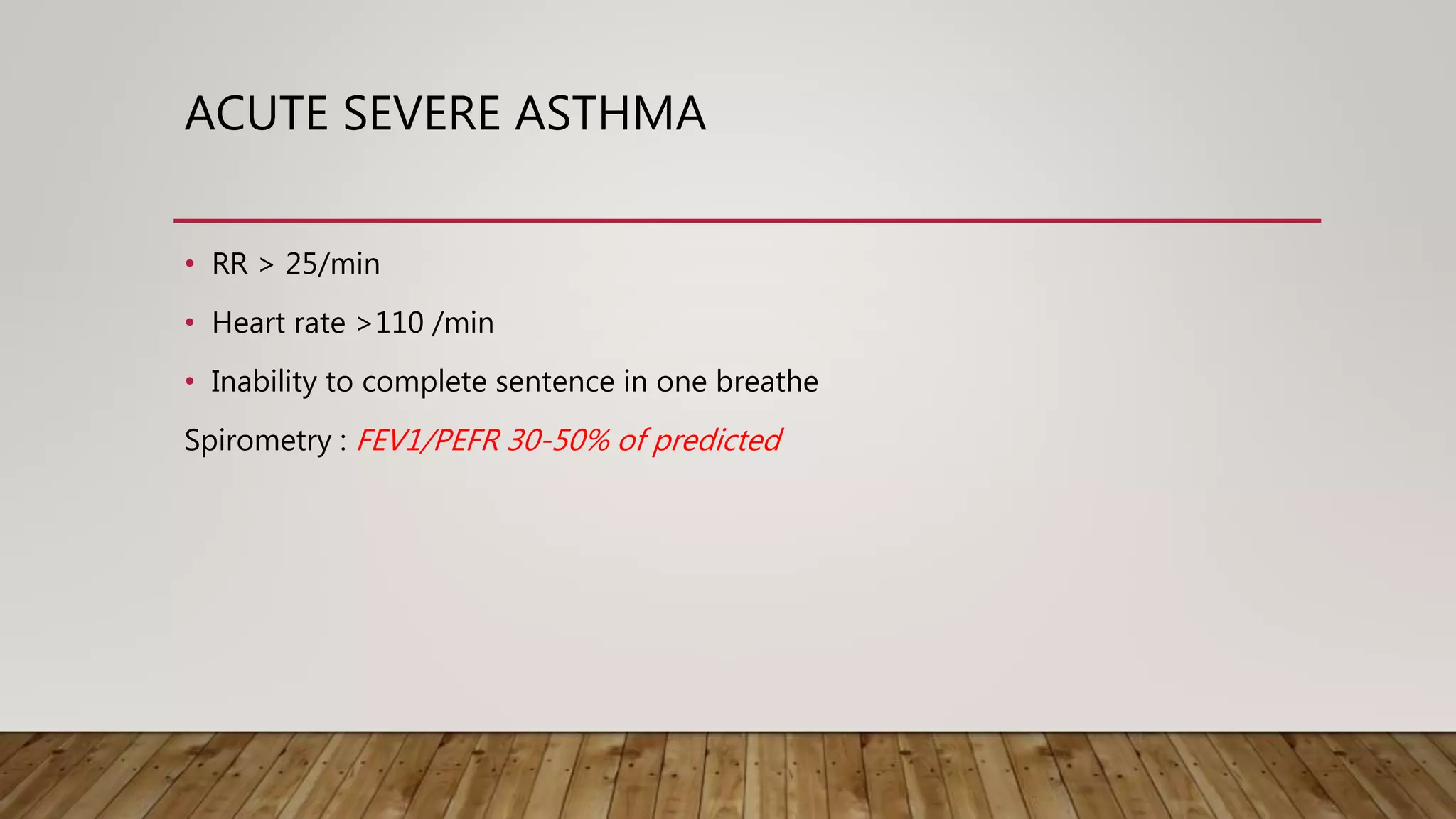
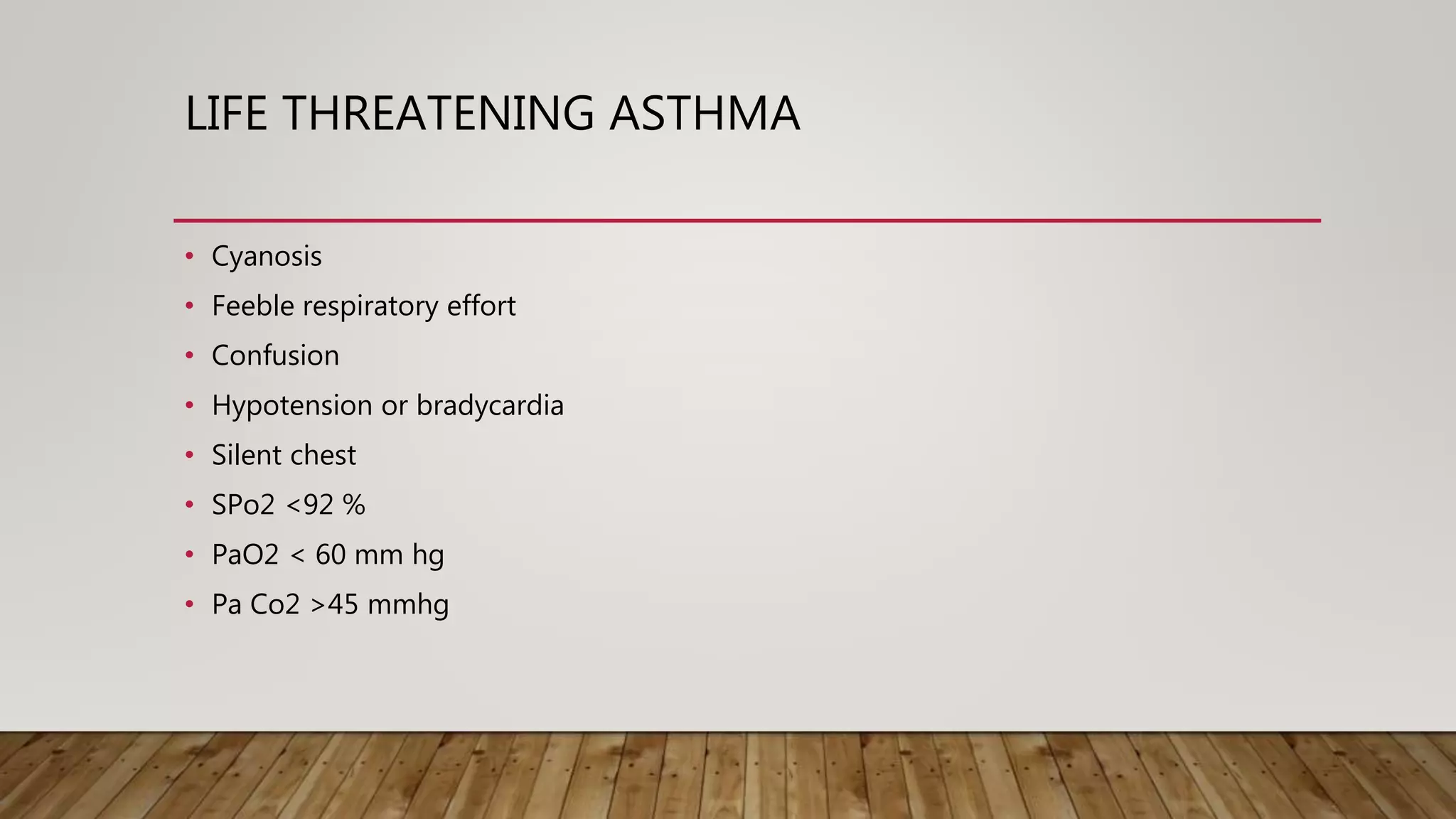
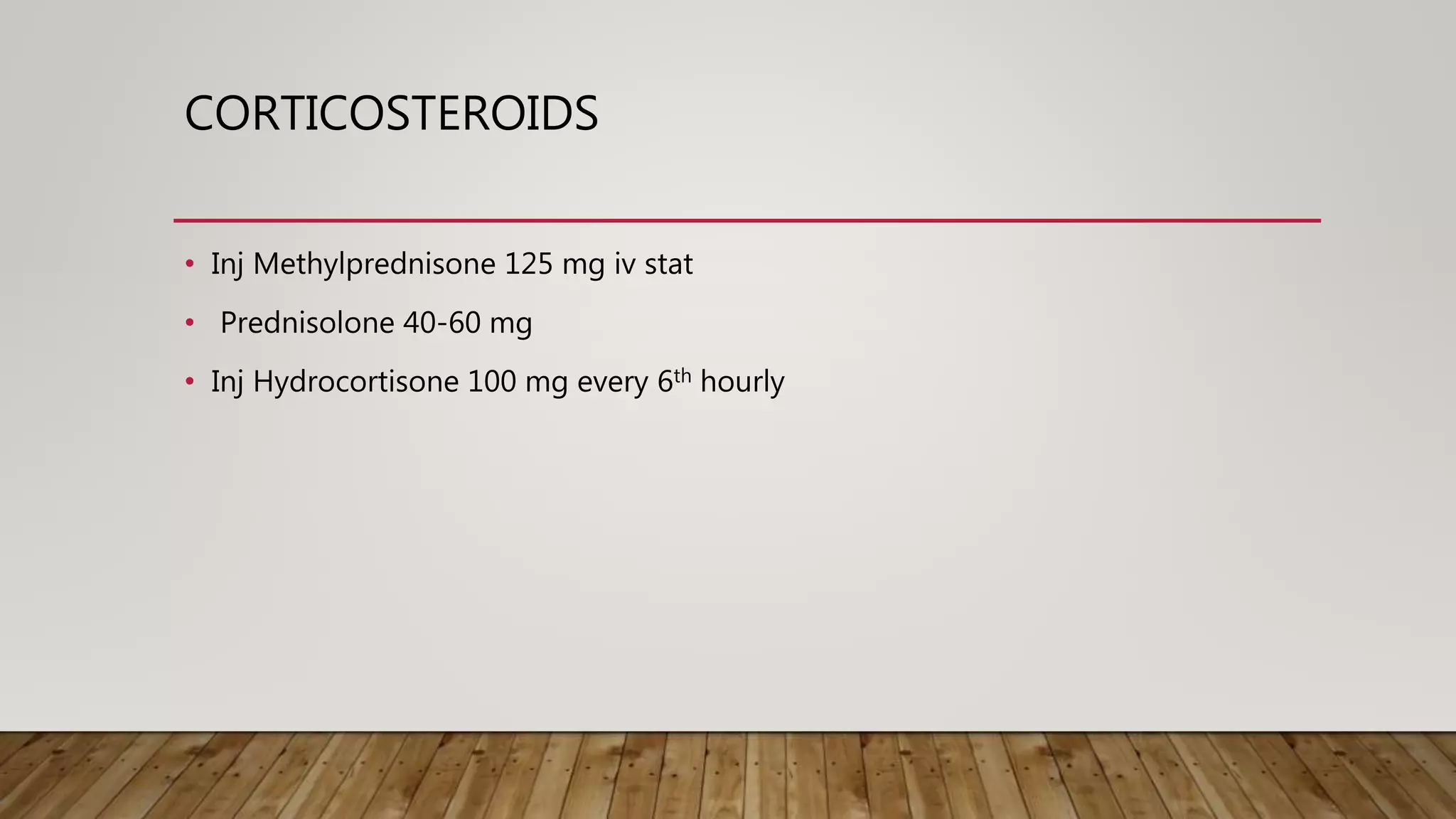
2. It provides definitions and levels of severity for acute asthma exacerbations from moderate to life-threatening. Clinical features, investigations and management are described.
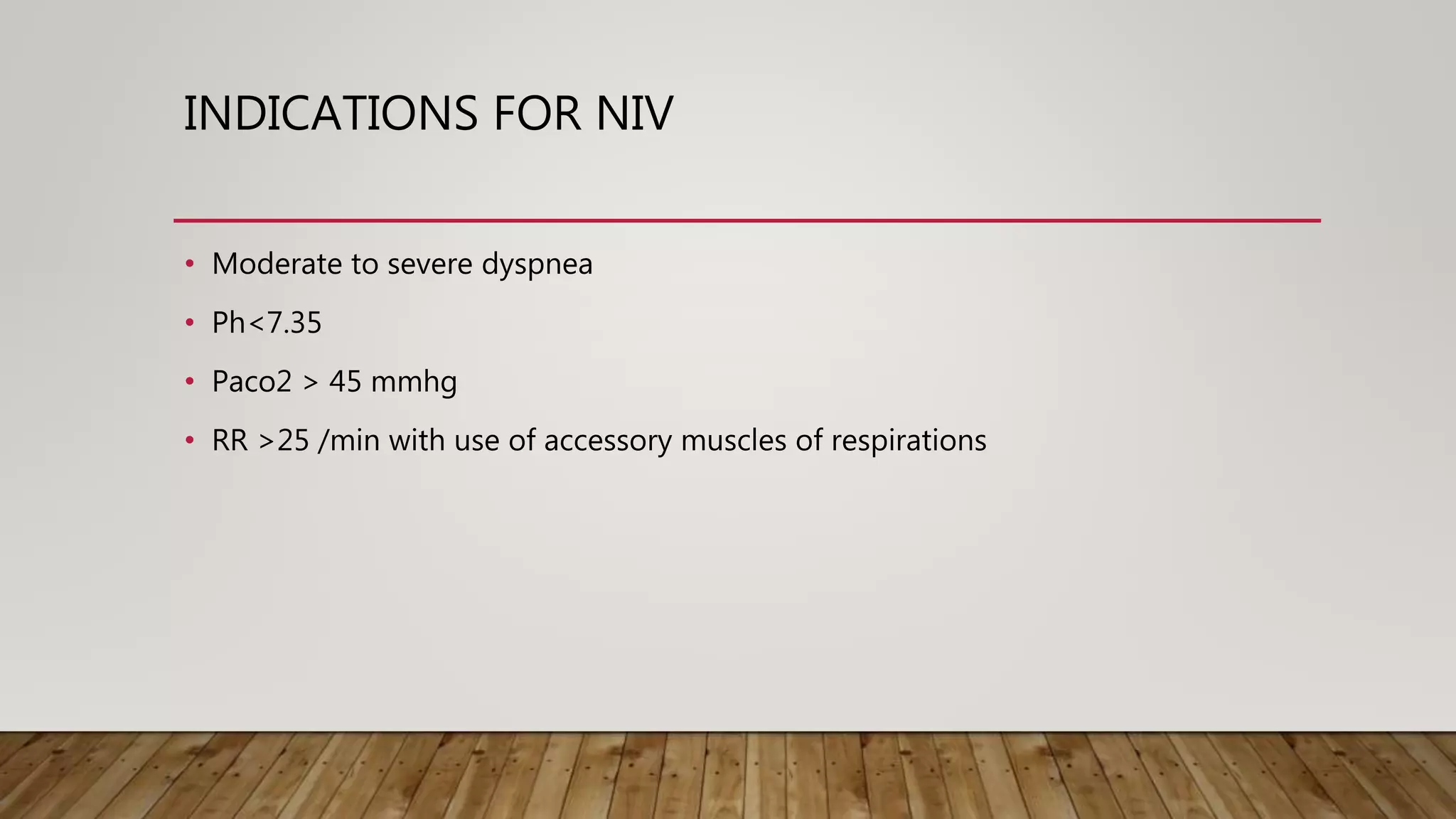
3. Acute exacerbation of COPD is also defined and precipitating factors, clinical features, investigations and treatment principles are outlined. Non-invasive ventilation criteria and contraindications are noted.