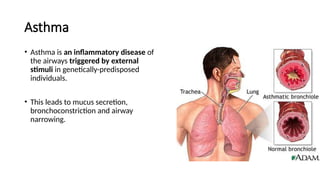
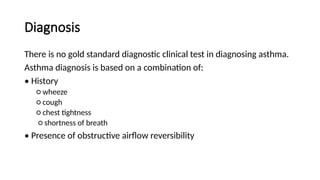
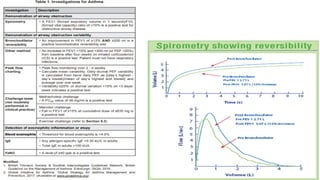
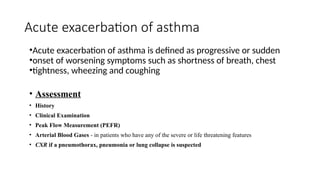
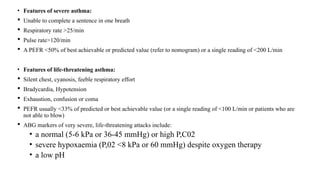
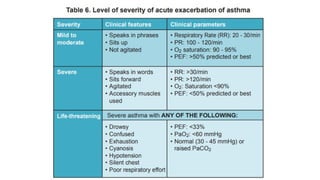
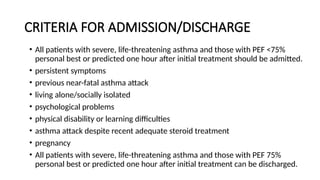
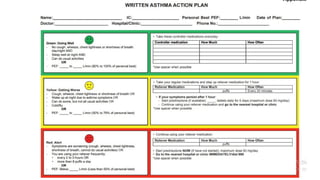
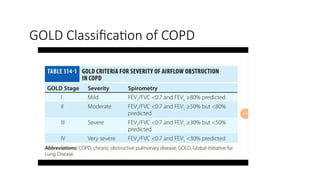
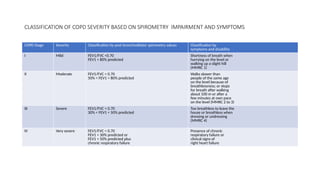
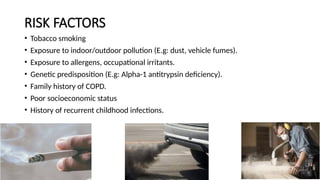
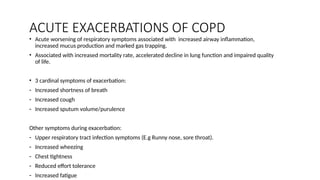
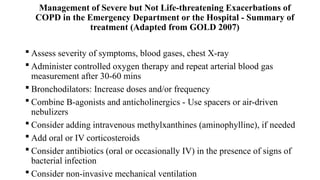
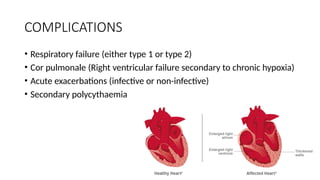
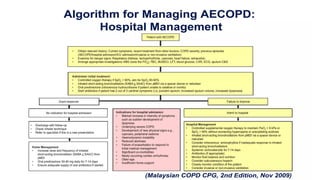
The document discusses asthma as an inflammatory airway disease characterized by symptoms such as wheezing and shortness of breath, with diagnosis based on clinical history and symptoms. Chronic obstructive pulmonary disease (COPD) is described as a progressive condition with airflow limitation that is generally irreversible, classified by severity based on spirometry and symptoms. Both conditions involve acute exacerbations and significant management strategies, including medication and assessment of severity.