The document provides information on the anatomy, physiology, and congenital disorders of the esophagus. It discusses:
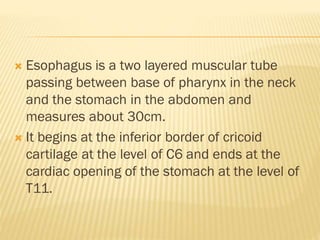
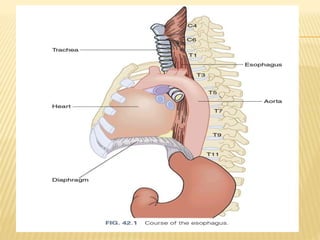
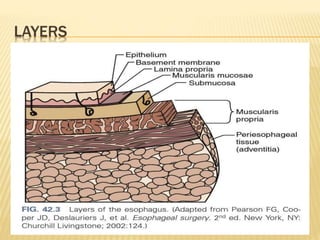
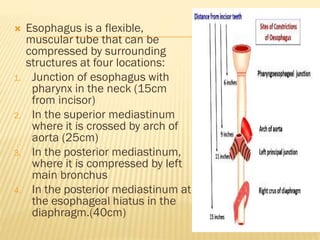
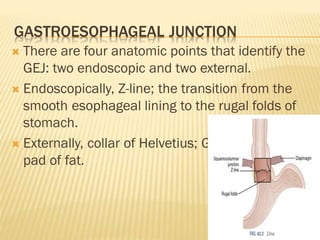
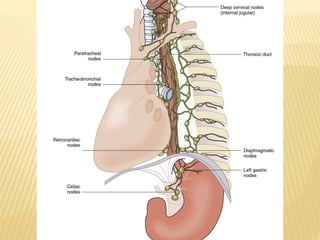
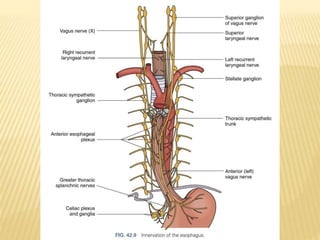
1. The esophagus is a muscular tube that connects the pharynx to the stomach. It has two sphincters and passes through the neck, thorax, and diaphragm.
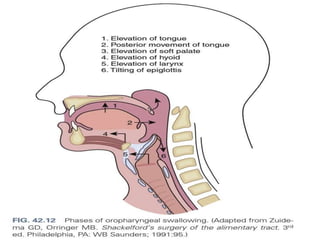
2. Swallowing involves three phases - oral, pharyngeal, and esophageal. In the esophageal phase, peristalsis propels food through the esophagus and into the stomach.
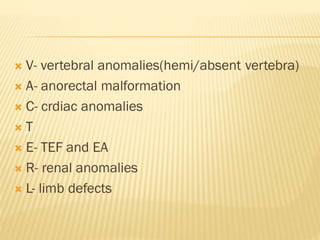
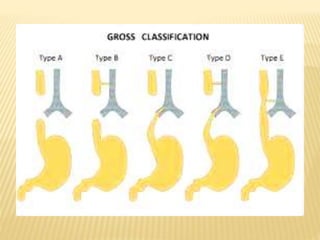
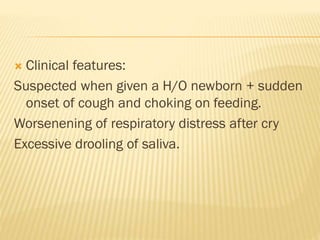
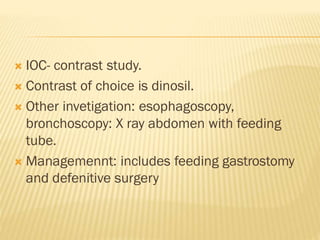
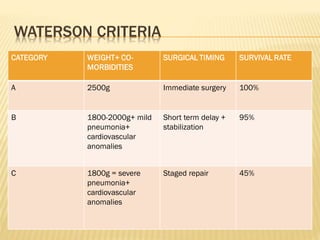
3. Congenital disorders include esophageal atresia and tracheoesophageal fistula, which involves an abnormal connection between the esophagus and trachea. Management