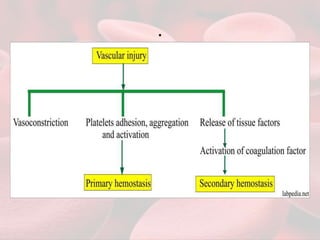
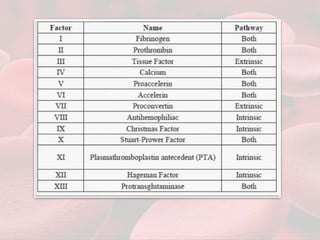
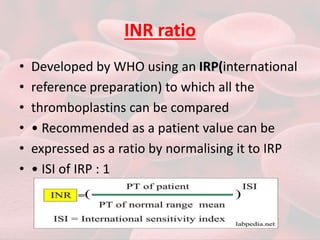
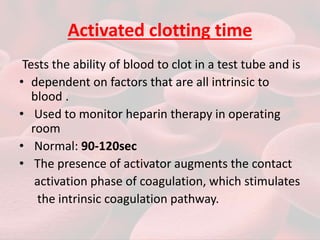
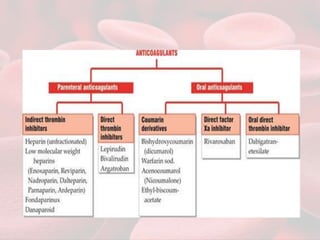
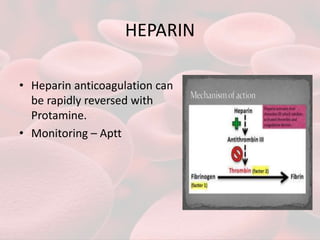
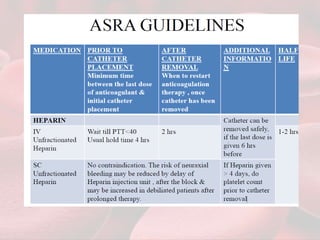
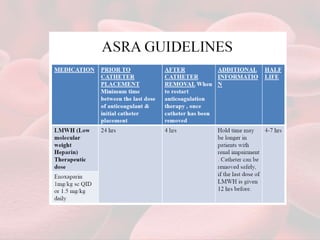
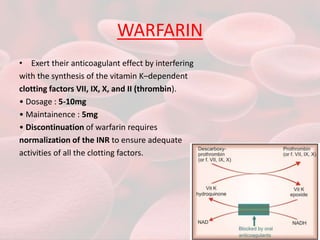
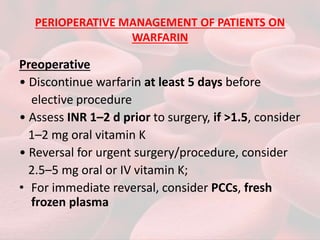
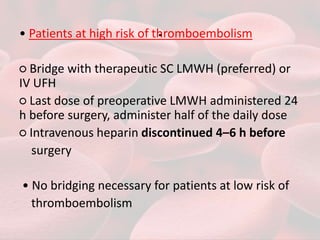
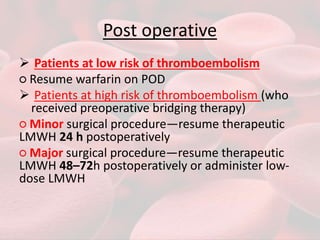
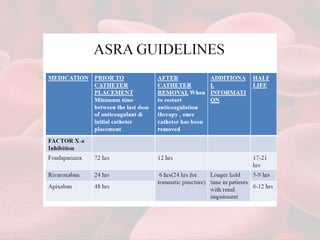
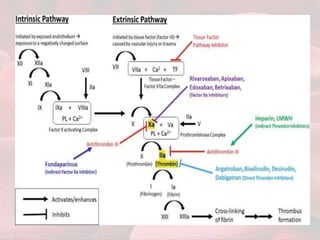
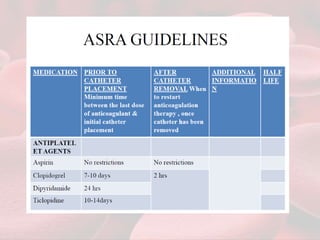
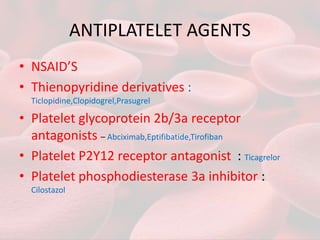
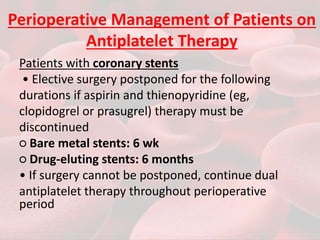
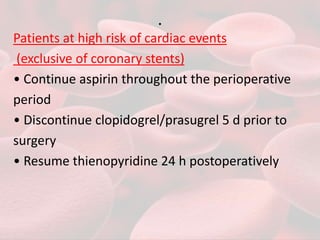
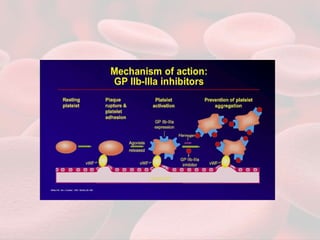
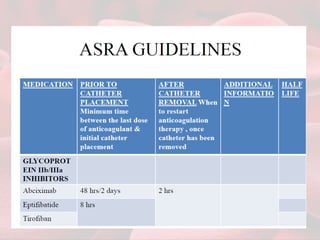
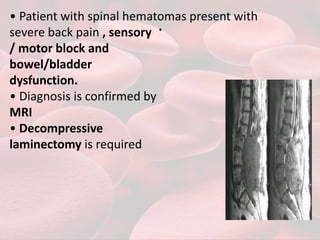
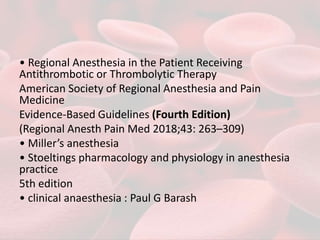
This document summarizes guidelines for providing regional anesthesia to patients taking anticoagulants or antiplatelet drugs. It discusses tests for evaluating primary hemostasis and coagulation, including platelet count, bleeding time, prothrombin time, partial thromboplastin time, and thrombin time. Common anticoagulants and antiplatelet drugs like heparin, warfarin, aspirin, and clopidogrel are described. Risks of regional anesthesia are outlined for different INR levels on warfarin. Perioperative management strategies for bridging anticoagulation and stopping/restarting various drugs before and after surgery are provided.