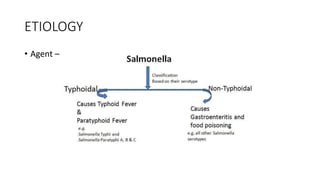
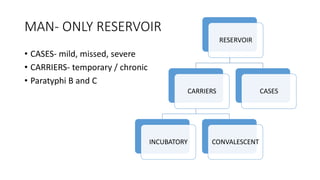
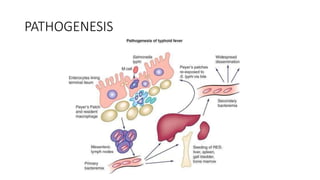
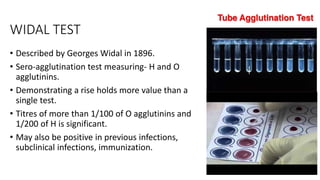
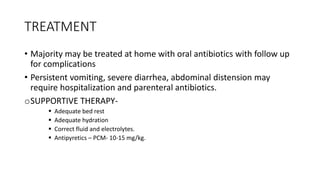
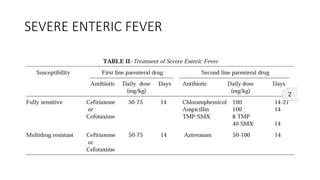
Enteric fever is caused by Salmonella Typhi and Paratyphi bacteria. It is a major health problem globally with over 21 million cases reported annually, especially in India. The bacteria are transmitted through contaminated food or water via the fecal-oral route. Clinical features include fever, abdominal pain, and complications like intestinal bleeding or perforation. Diagnosis involves blood or stool culture and serological tests. Treatment involves antibiotics and supportive care. Prevention focuses on hand washing, water treatment, and vaccination.