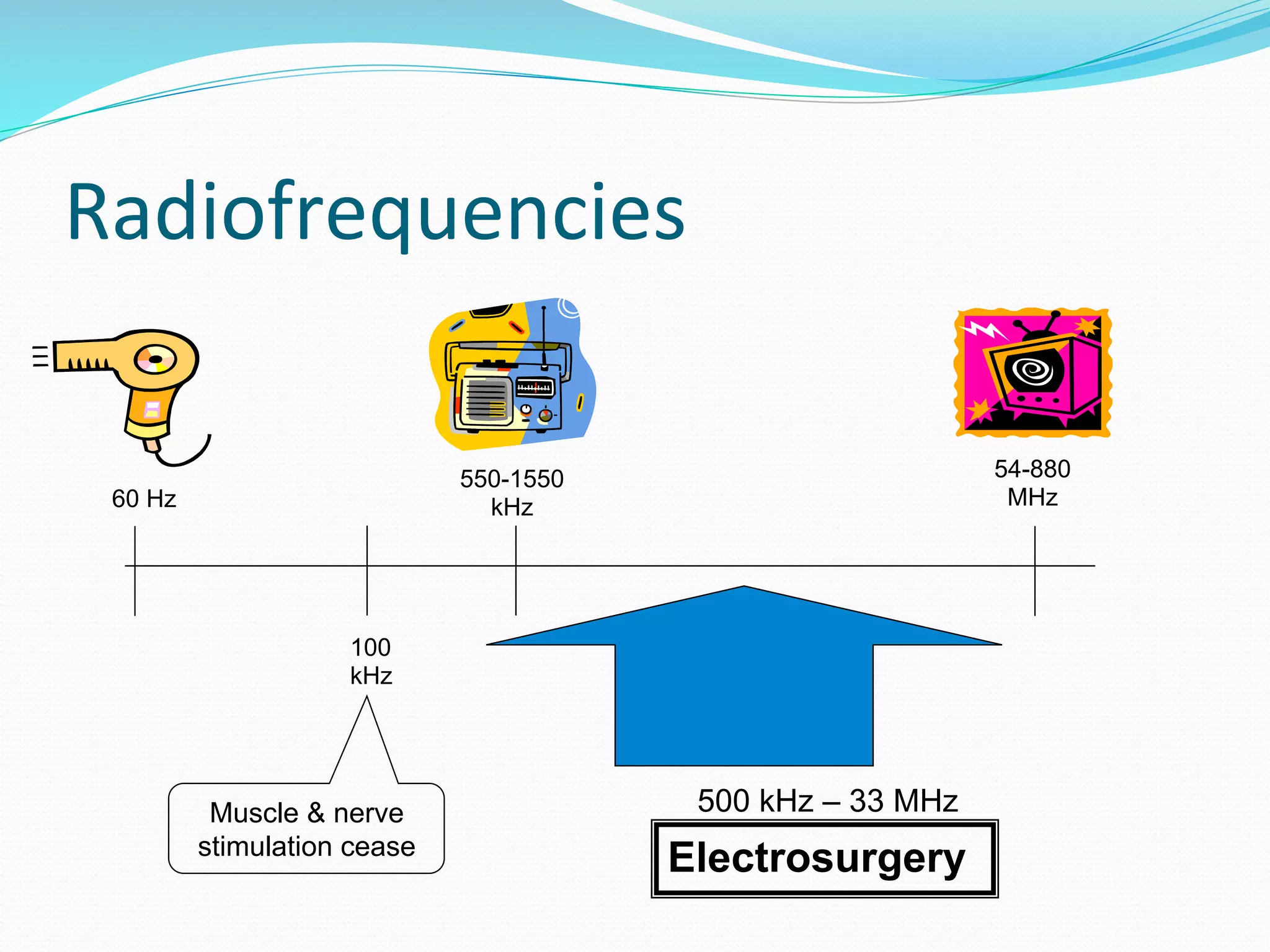
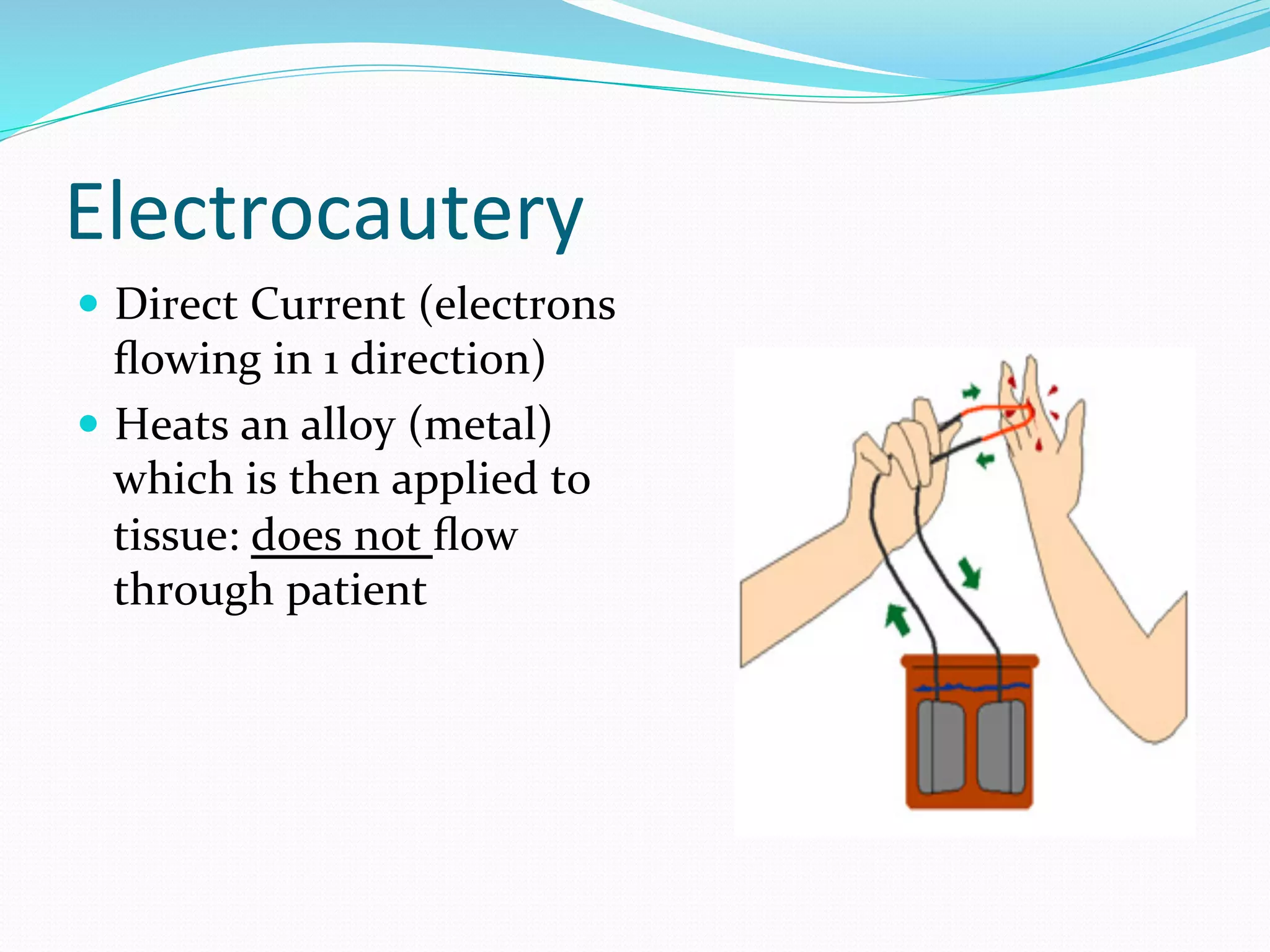
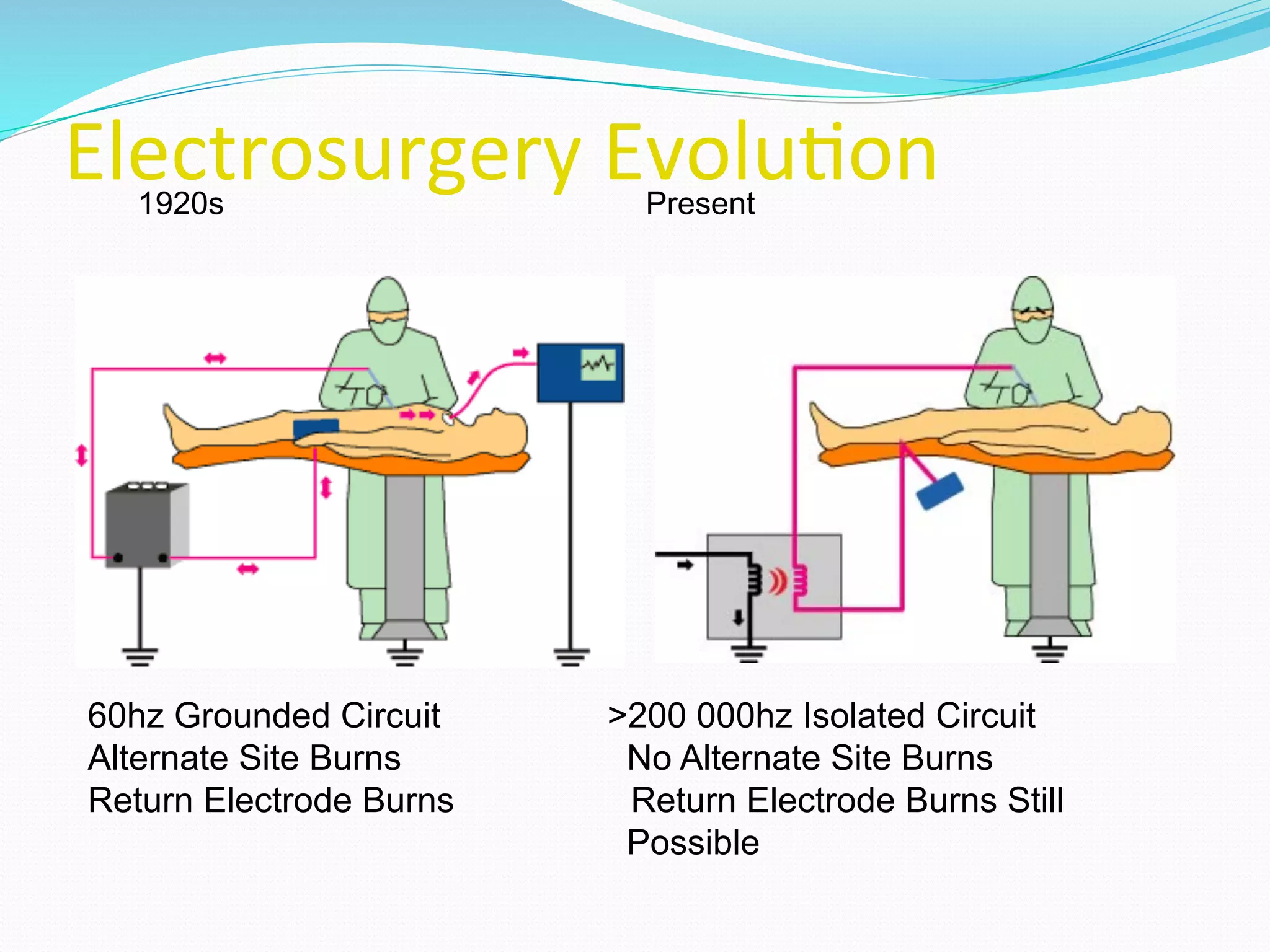
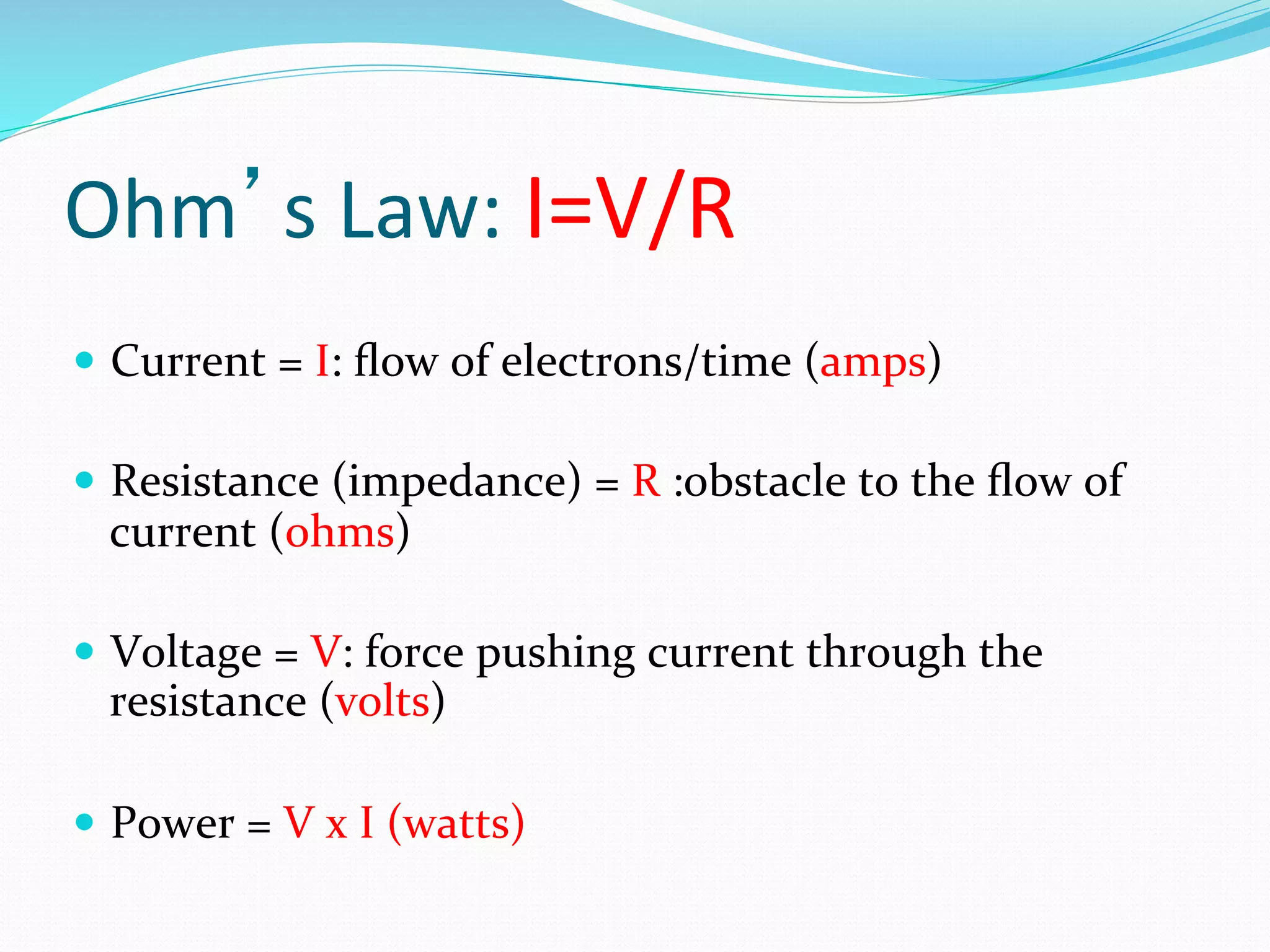
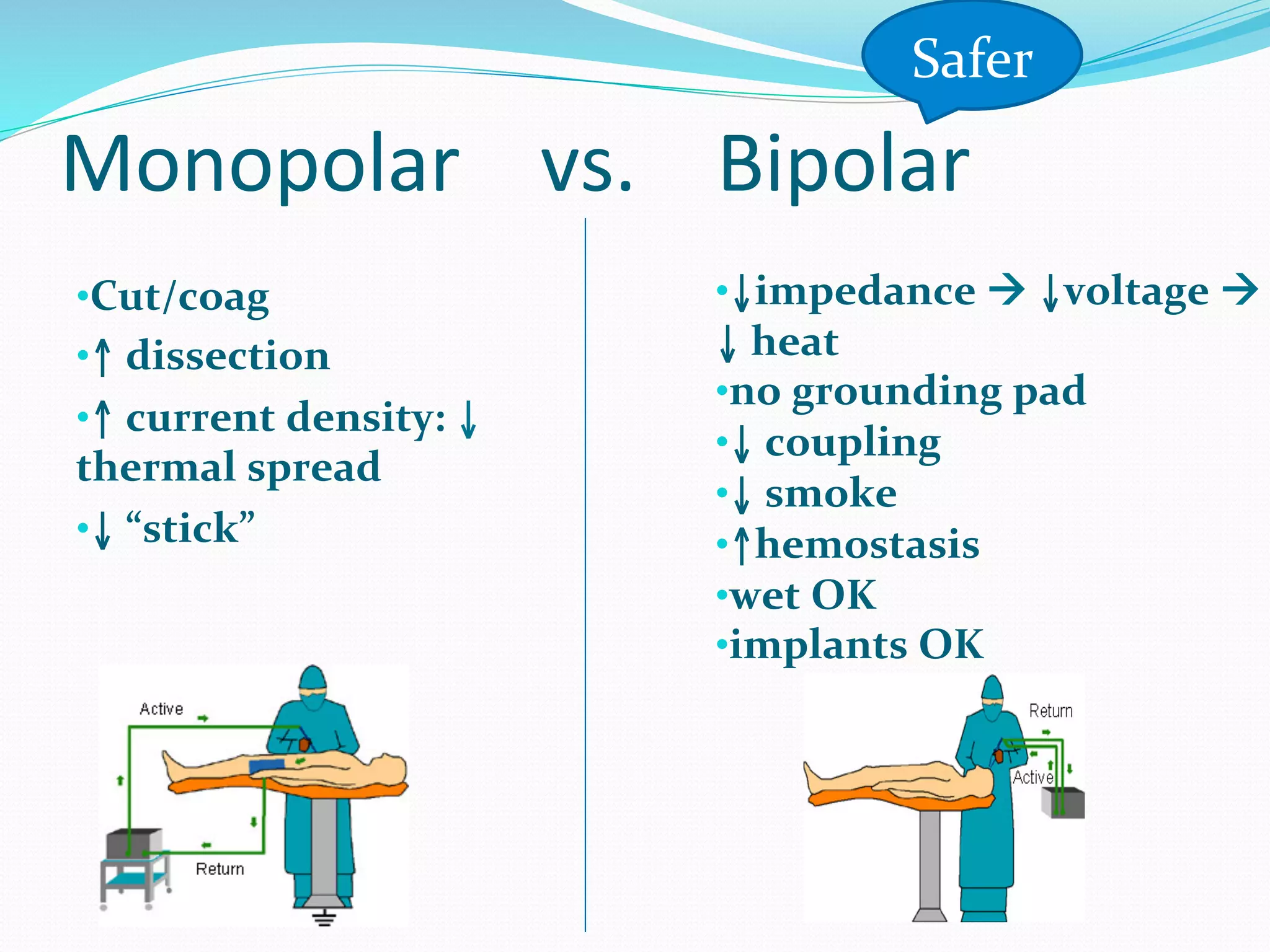
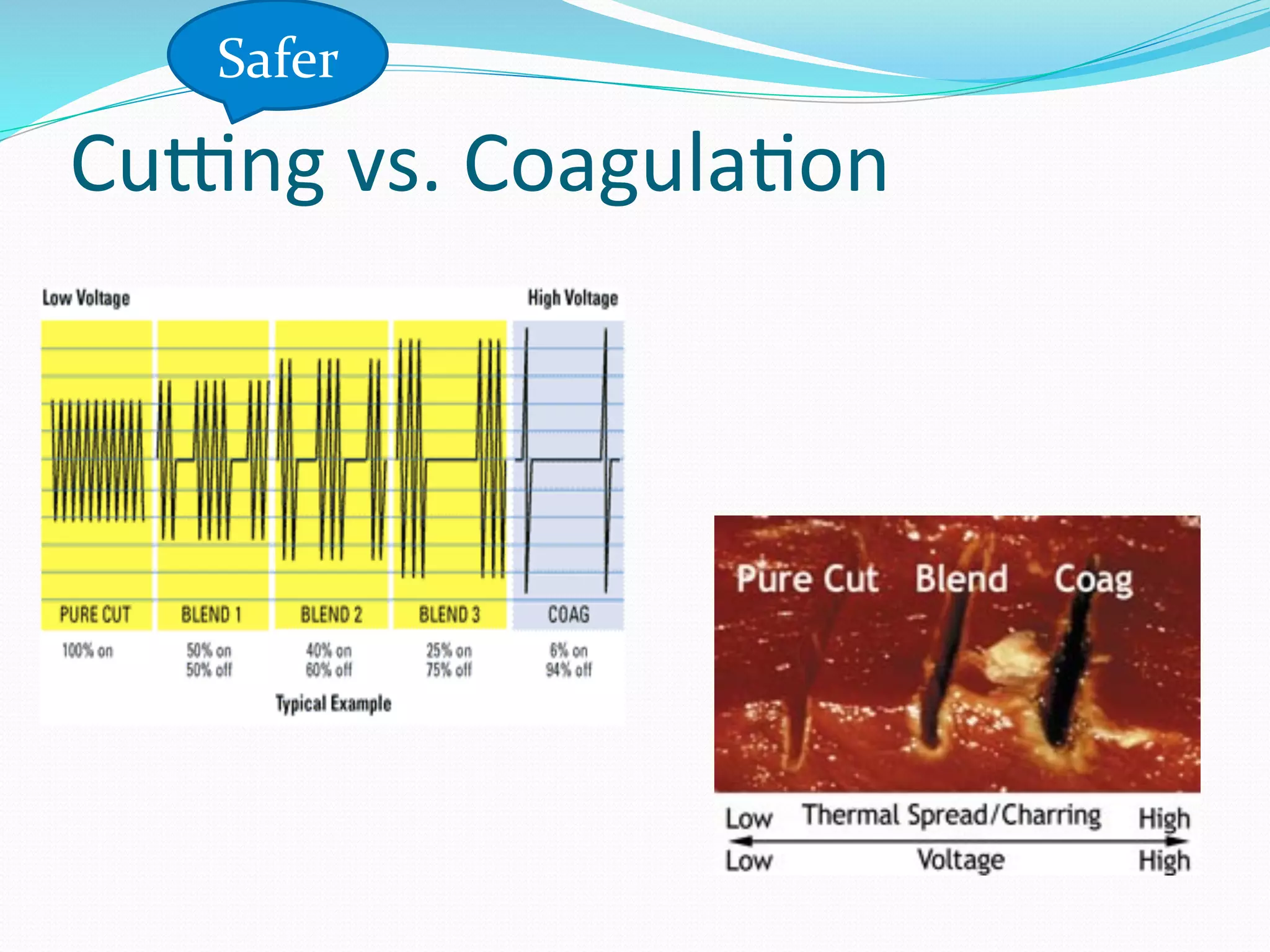
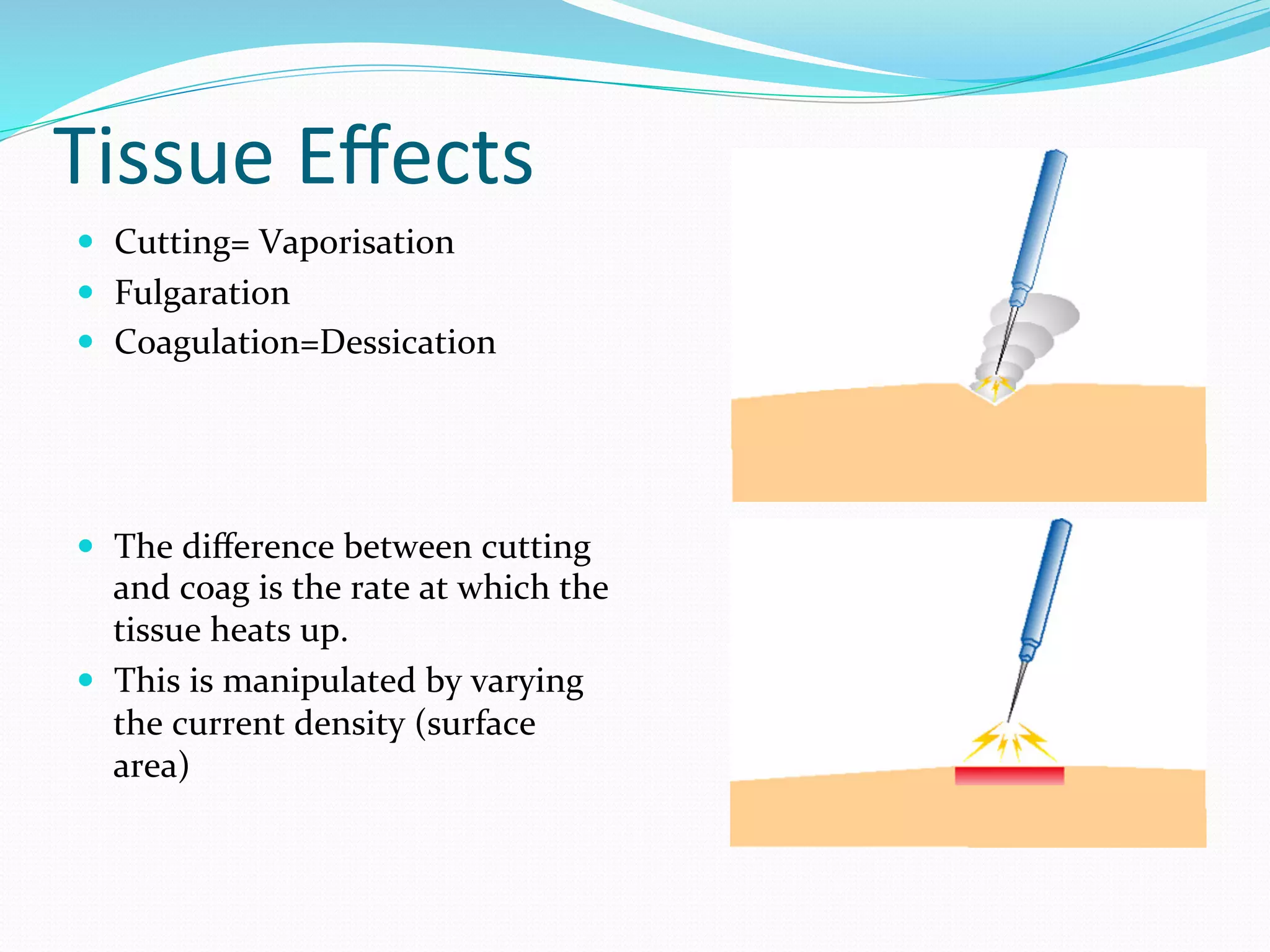
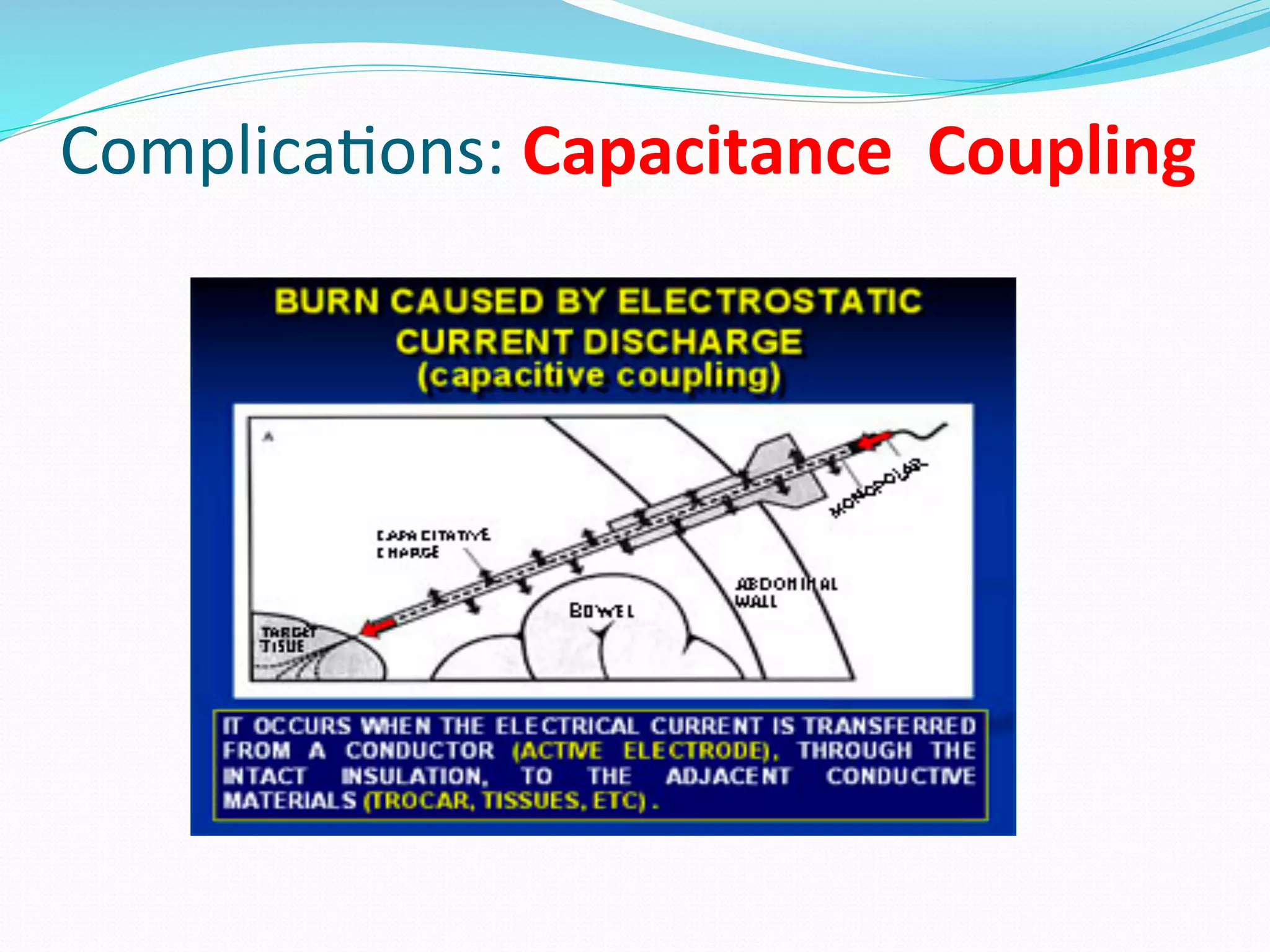
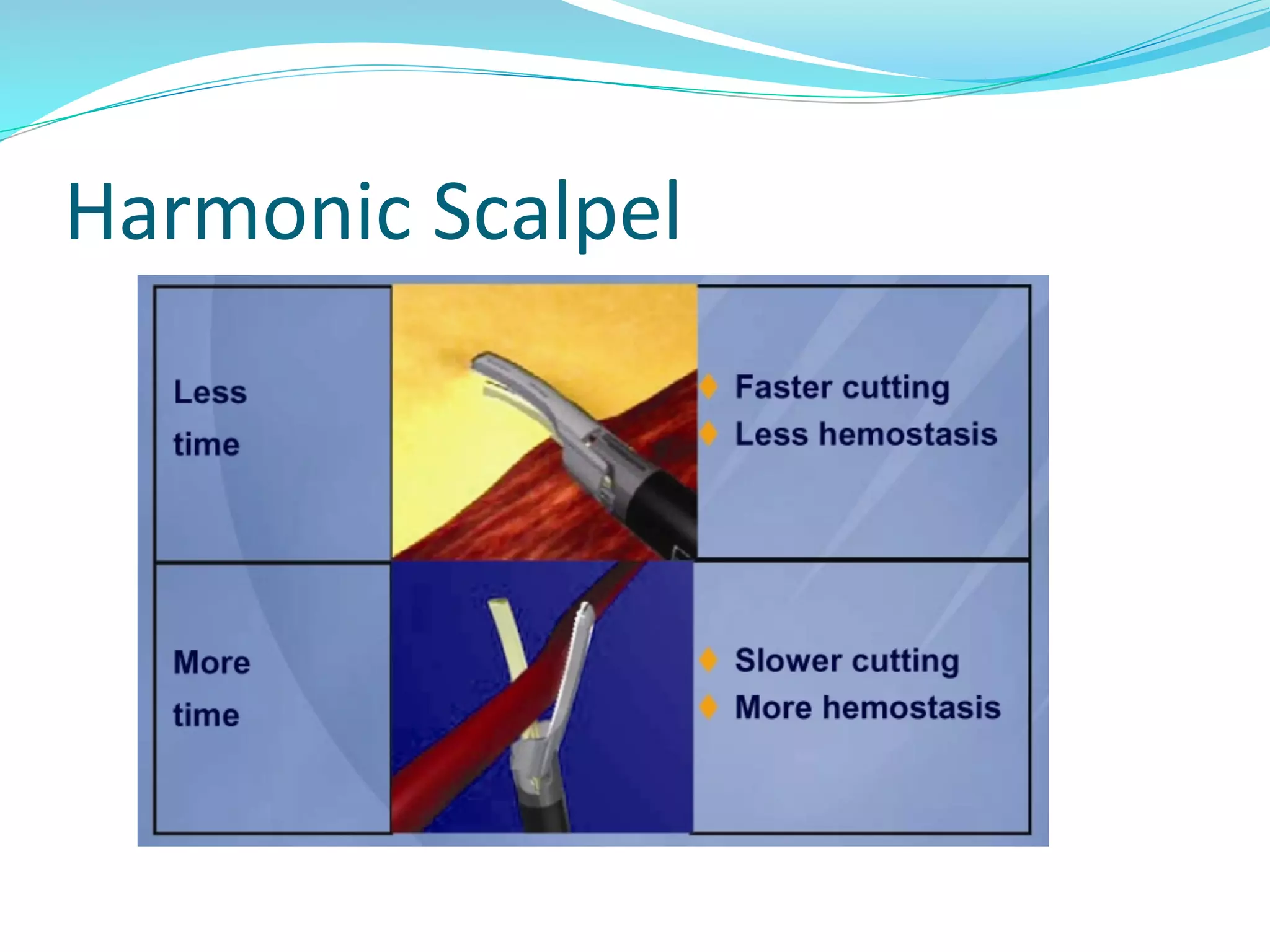
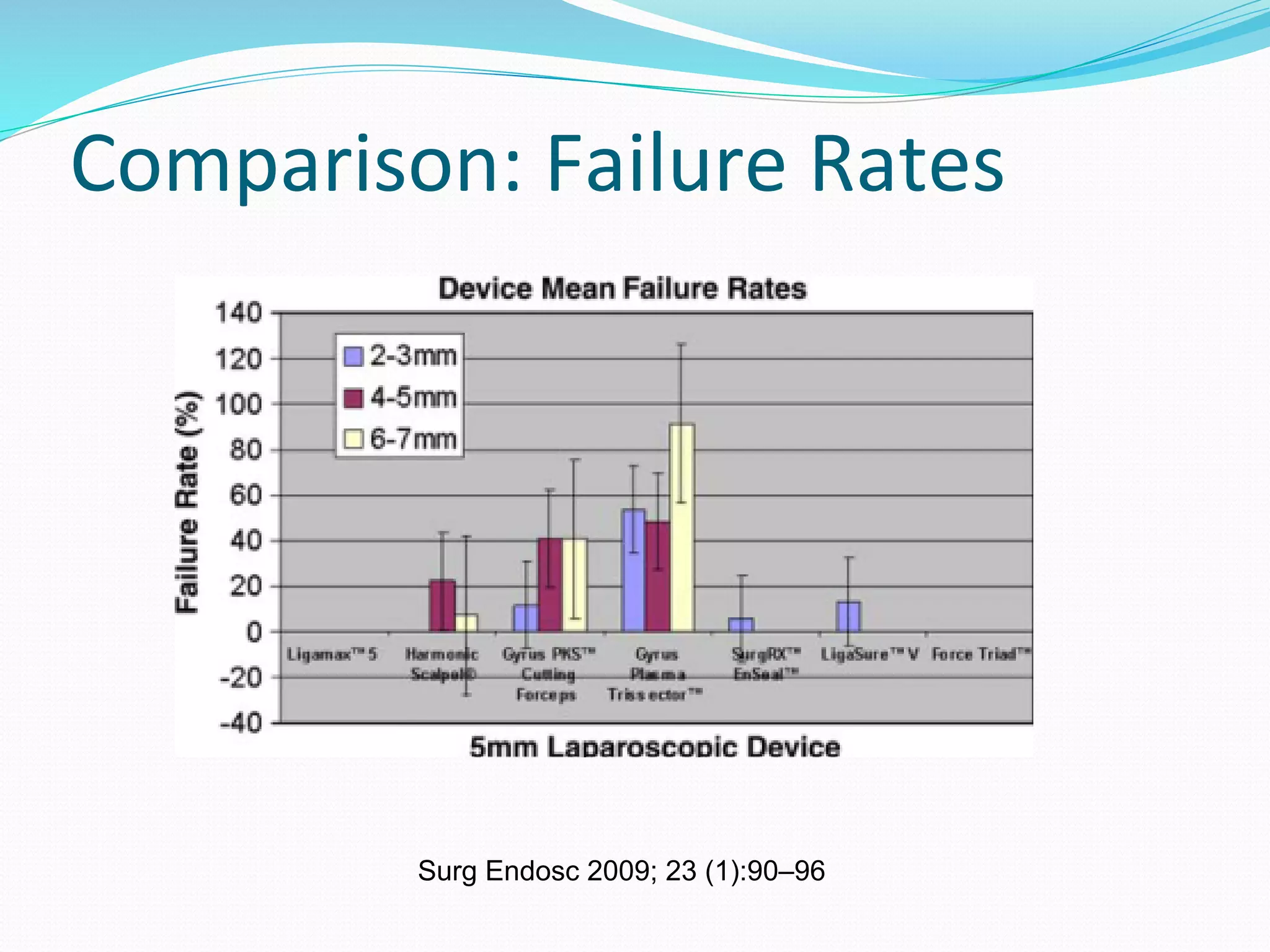
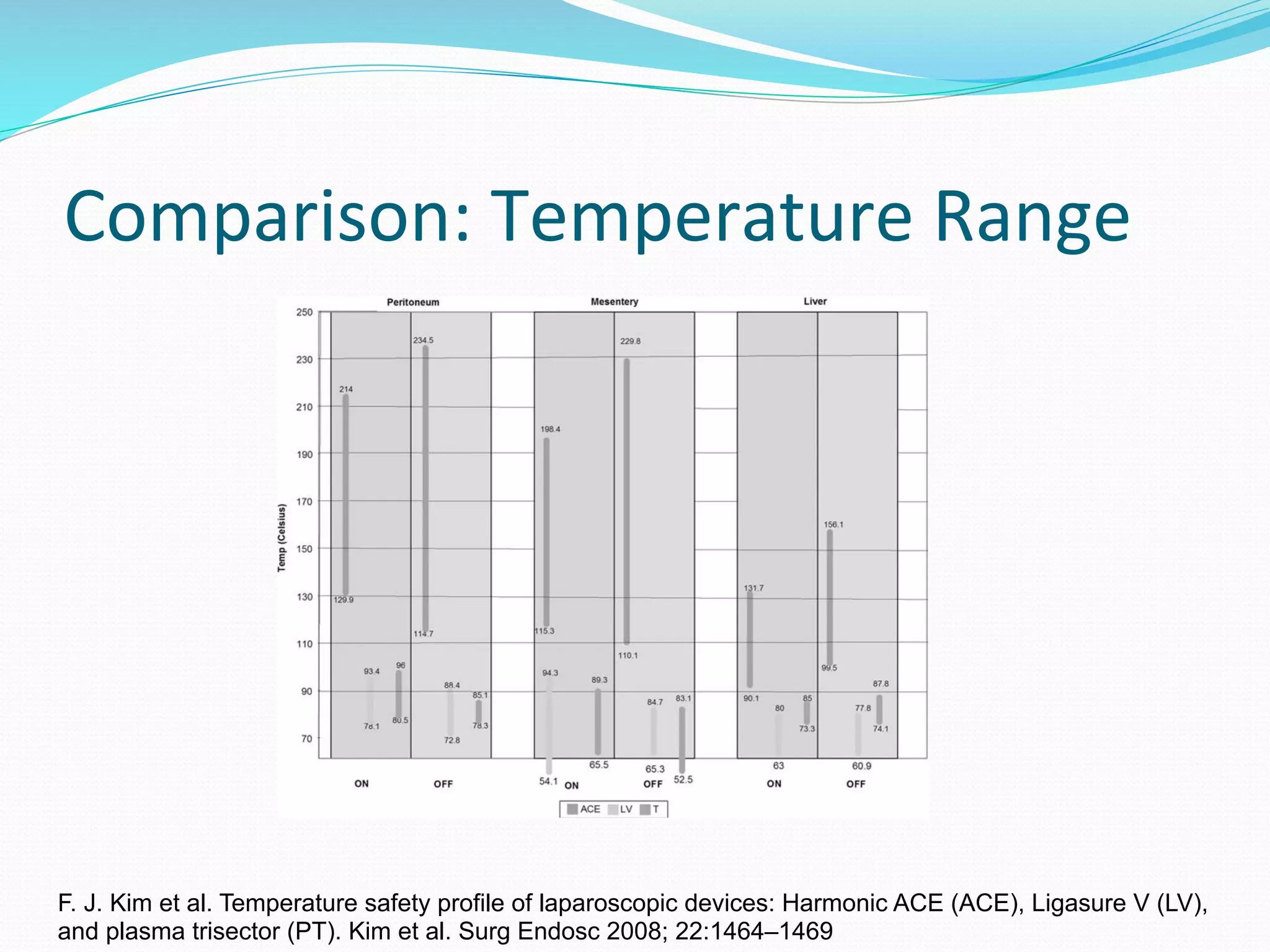
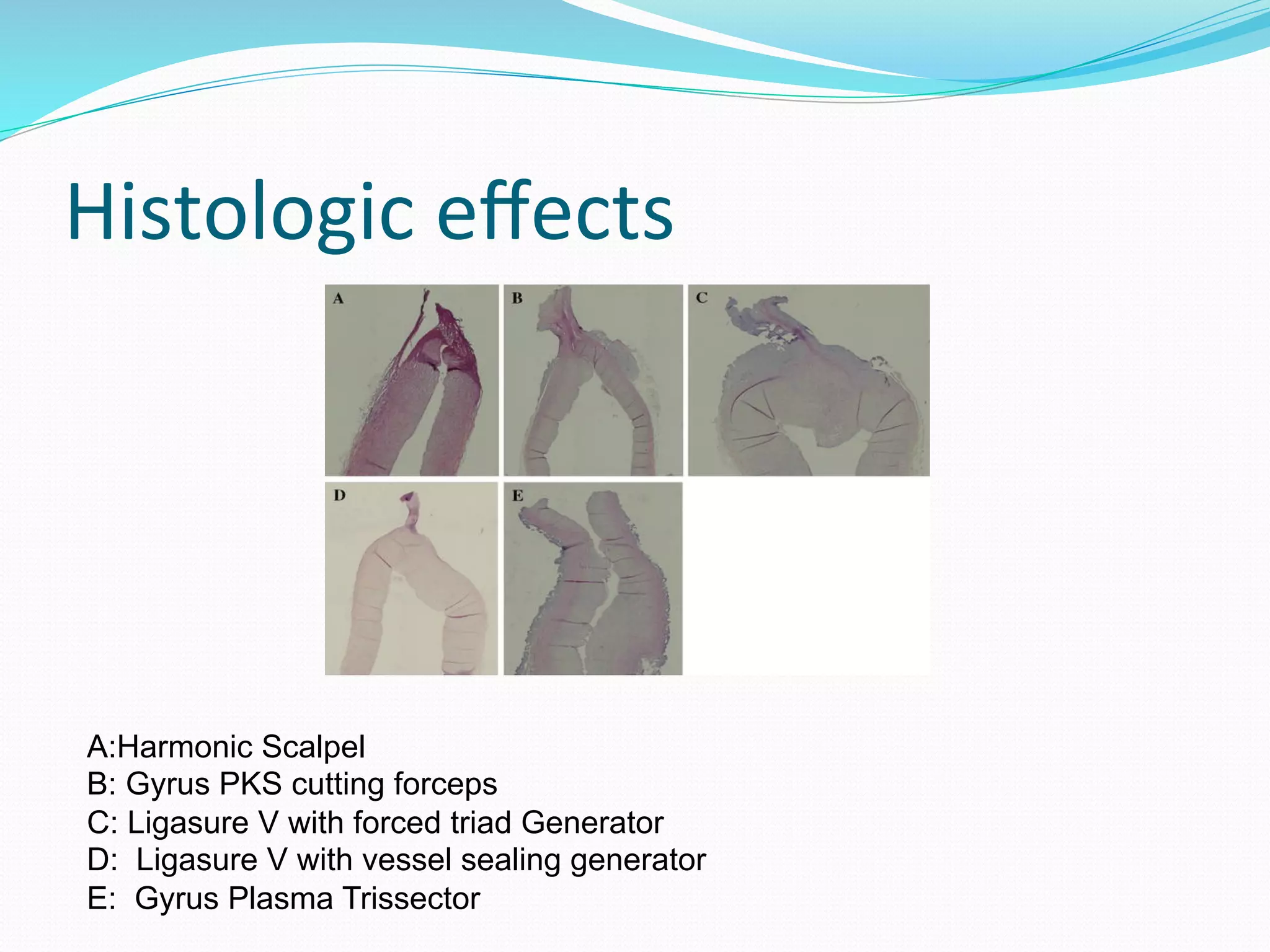
This document provides information on various techniques and technologies used in electrosurgery. It discusses the history and evolution of electrosurgery from the 1920s to present. Key aspects covered include the differences between electrocautery, electrosurgery, monopolar vs bipolar methods, and tissue effects. Complications are reviewed. Newer energy sources and technologies are introduced, such as advanced bipolar devices from Gyrus ACMI, Ethicon Endo-Surgery, and Covidien.