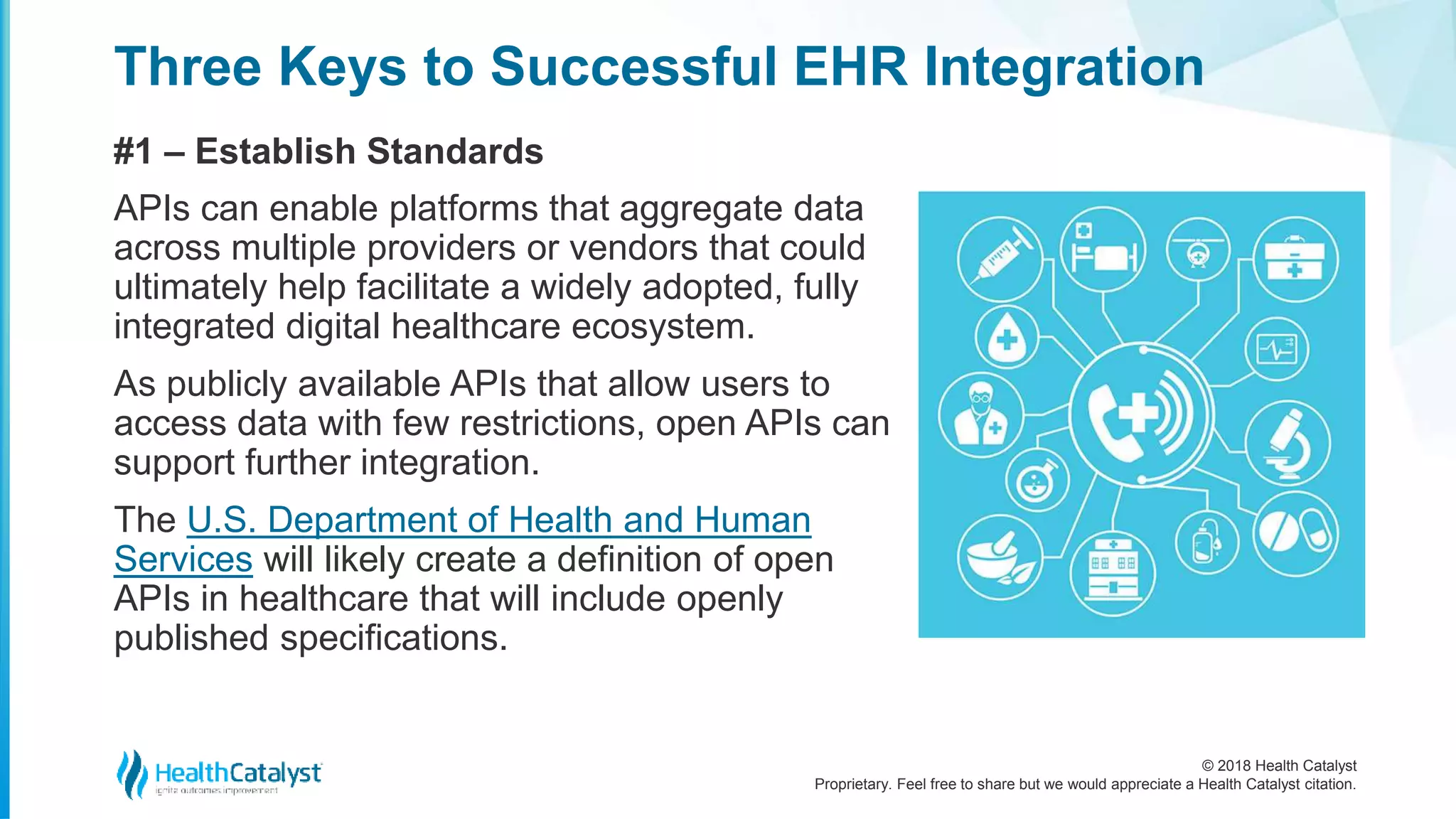
The document discusses the increasing need for Electronic Health Record (EHR) integration as digital health technology adoption is projected to exceed $379 billion by 2024. It highlights the importance of interoperability to leverage data from various digital health tools for improved patient care, while also addressing existing technical and administrative challenges to integration. The document outlines key steps for successful EHR integration, including establishing standards, achieving functional integration, and developing relevant use cases.