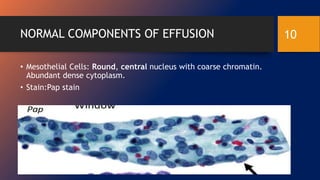
This document discusses effusion cytology, including the types and sampling of serous effusions. Serous effusions can occur in the pleural, peritoneal, and pericardial cavities and can be transudates or exudates. Transudates have little protein and few cells while exudates are rich in protein and cells. Effusions are usually sampled via thoracentesis, paracentesis, or pericardiocentesis. Normal components in effusions include mesothelial cells, histiocytes, lymphocytes, and collagen balls. Neoplastic effusions may contain malignant cells and have a more sudden onset than non-neoplastic effusions which are devoid of cancer cells.