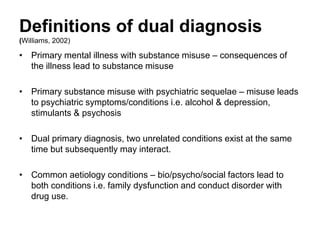
This document discusses dual diagnosis, which refers to co-occurring mental health and substance use disorders. It provides definitions of dual diagnosis from medical taxonomy and from Williams, who describes four types: primary mental illness leading to substance use; primary substance use leading to psychiatric issues; dual primary diagnoses occurring simultaneously; and common etiological factors leading to both. The document analyzes four case studies according to Williams' definitions and provides recommendations for practitioners, including engagement, assessment, avoiding assumptions, optimism, harm reduction, information sharing, and multi-agency collaboration.