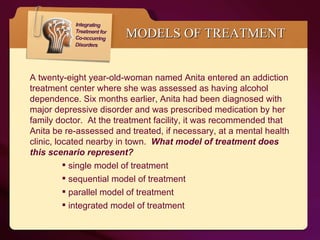
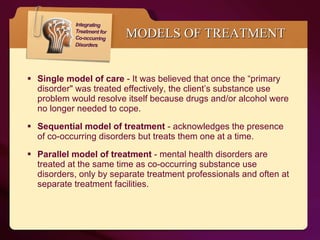
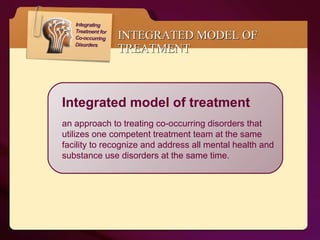
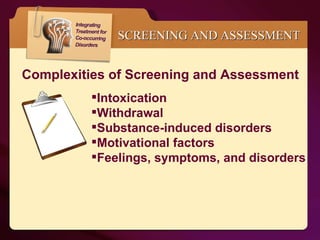
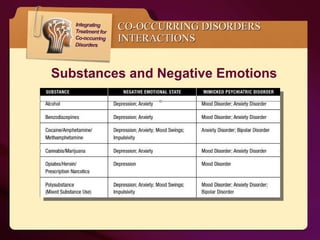
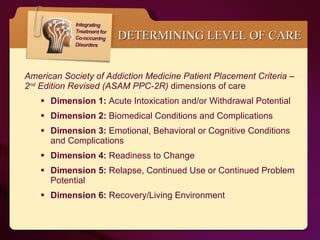
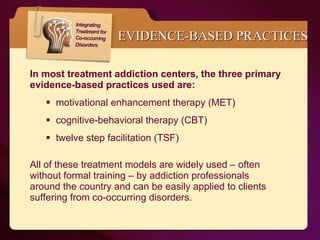
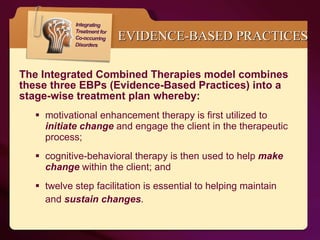
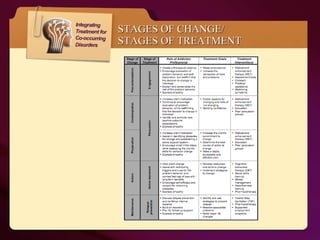
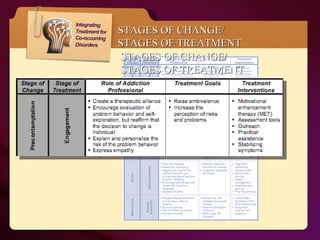
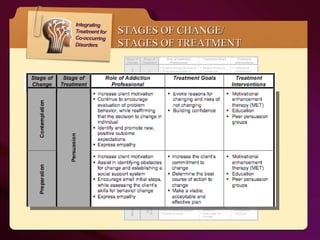
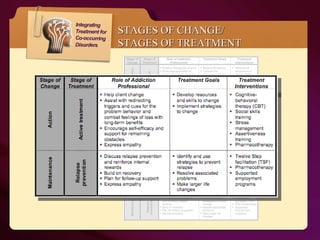
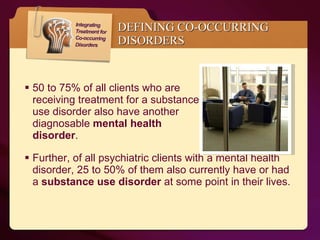
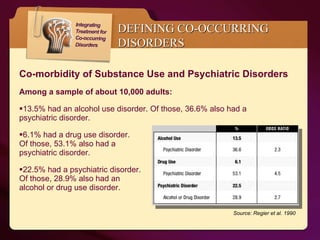
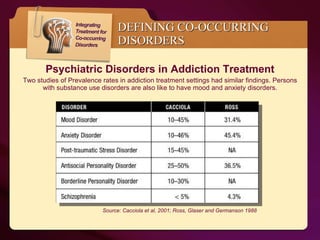
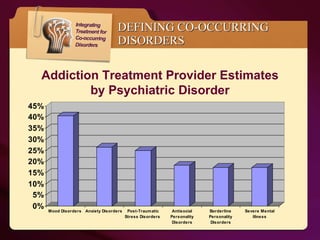
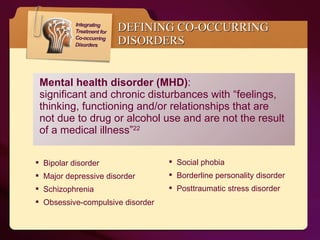
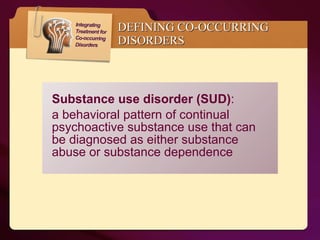
This document discusses a web conference on treating co-occurring disorders. It defines co-occurring disorders as the simultaneous existence of substance use disorders and mental health disorders. Approximately 50-75% of those with substance use disorders also have a mental health disorder. The document contrasts traditional treatment models with integrated treatment and argues that integrated treatment, which addresses both disorders simultaneously with one treatment team, has benefits over other models. It provides information on screening and assessment tools, levels of care, and evidence-based therapies for treating co-occurring disorders.




![Co-occurring disorders (COD) : the simultaneous existence of “one or more disorders relating to the use of alcohol and/or other drugs of abuse as well as one or more mental [health] disorders.” 18 DEFINING CO-OCCURRING DISORDERS](https://image.slidesharecdn.com/web07142-110808205257-phpapp01/85/Integrated-Treatment-for-Co-occurring-disorders-19-320.jpg)