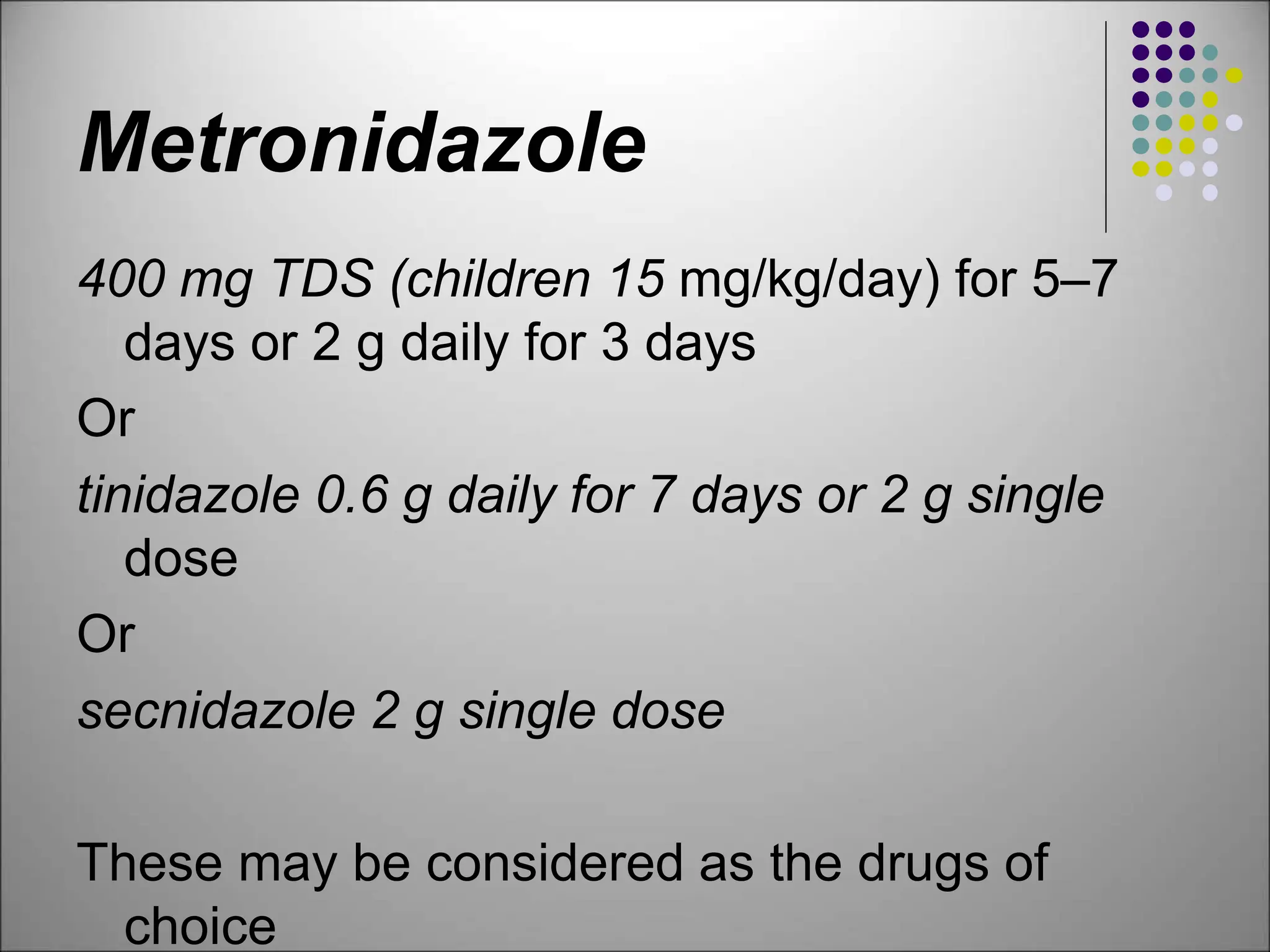
The document discusses various antiamoebic drugs used to treat amoebiasis caused by Entamoeba histolytica, highlighting their classifications, mechanisms of action, and adverse effects. Metronidazole is identified as the primary treatment, effective against multiple protozoa, with alternative medications like tinidazole and secnidazole also noted. Additionally, the document includes information on pharmacokinetics, contraindications, and treatment regimens for related infections.