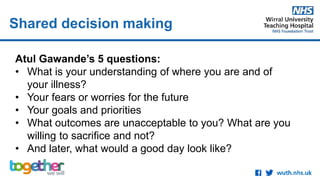
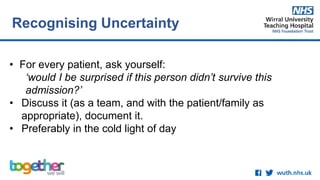
The document discusses the importance of shared decision making in treating patients with advanced diseases such as malignant bowel obstruction. It highlights various approaches to patient communication and the role of palliative care teams in managing treatment options, including the consideration of parenteral nutrition. Additionally, it outlines the complexities of cancer-cachexia syndrome and the multidisciplinary approach required for optimal patient care.