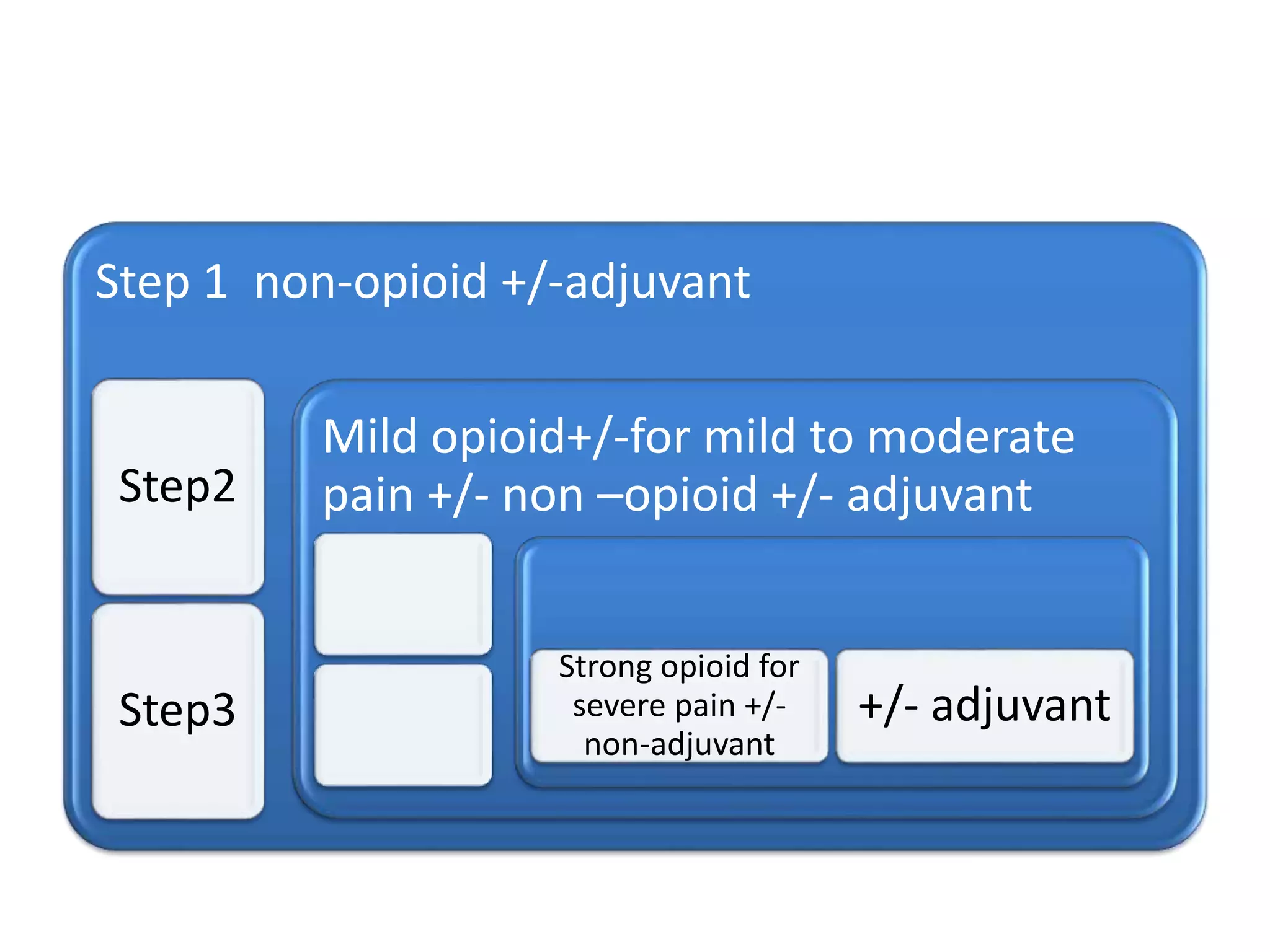
This document discusses palliative care, which aims to improve quality of life for patients facing life-threatening illnesses. It defines palliative care as preventing and relieving suffering through early assessment and treatment of pain and other problems. The goals of palliative care are to relieve suffering, treat pain and distressing symptoms, and provide psychological, spiritual and social support. Common symptoms addressed in palliative care are discussed, including pain, nausea, vomiting, dyspnea, constipation and fungating wounds. The importance of psychological care and social support for patients and families is also outlined.