This document summarizes a study that explored nurses' experiences caring for patients over 65 years old who were receiving antibiotics. The study found that nurses play a pivotal role through their nursing practice, infection prevention efforts, and teamwork. Their close relationships with patients and awareness of "little changes" allow them to identify potential infections. Preventing antibiotic use when possible is important. The nurses emphasized the importance of communication, education, and collaboration between nurses and other staff to ensure optimal antibiotic use and care for older patients. The findings suggest nurses have valuable knowledge about antibiotic use in older adult settings that could inform nursing education, practice, and policies.
![HALT – matching the data
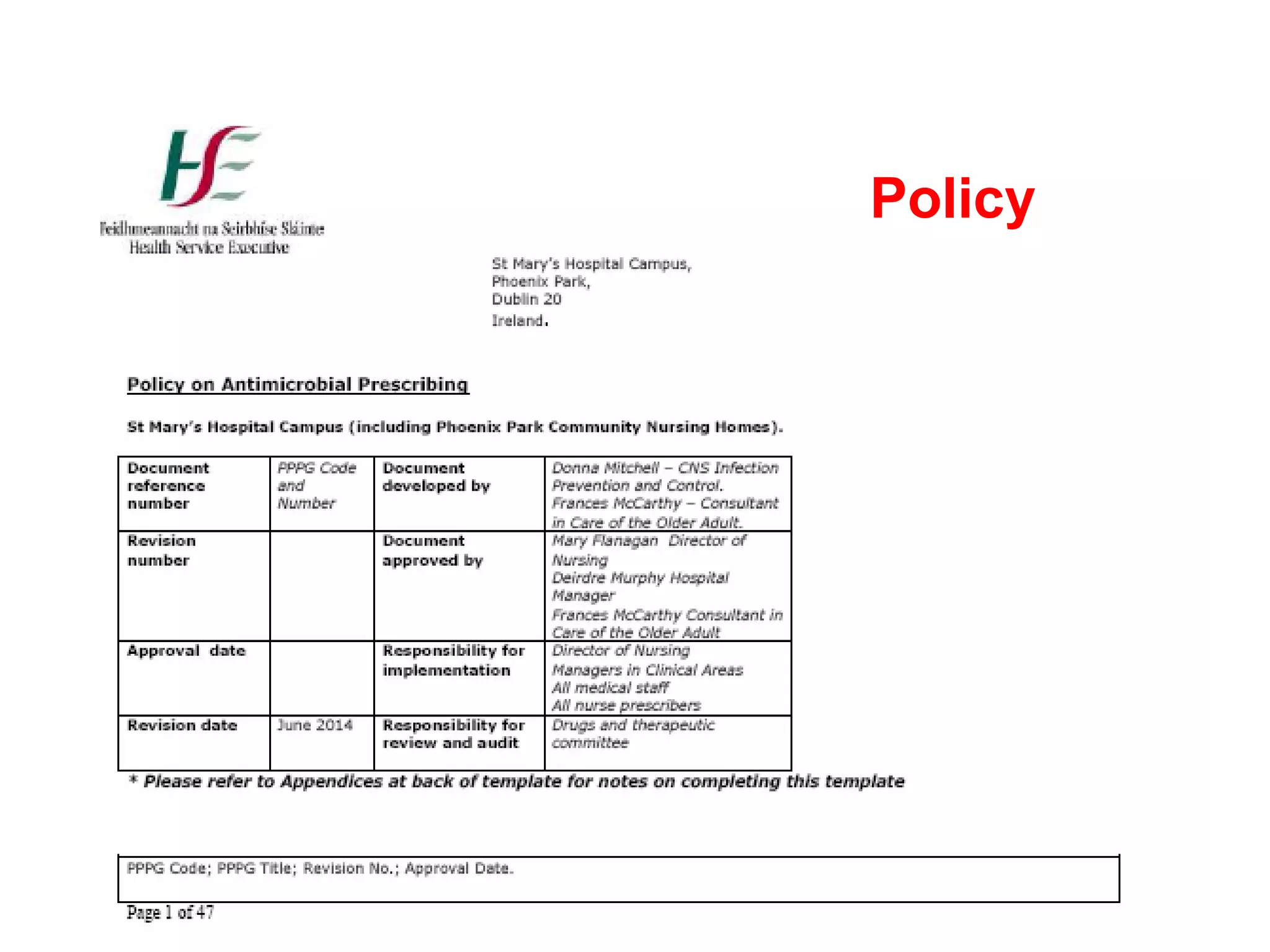
National:
• 5910 residents surveyed
ranging from 5 to 203
beds
• 5.0% had HCAI
• 9.5% prescribed
antimicrobials
• 62% had access to IPC
practitioner [76% of these
based off-site]
• GP care 43%, medical
staff employed 33%, both
in 24%.
St Mary’s:
• Larger scale bed size
• 1.6% had HCAI
• 4.3% prescribed
antimicrobials](https://image.slidesharecdn.com/donnamitchellnursesexperienceofantibioticuseinptsover65-131126074337-phpapp01/75/Donna-mitchell-nurses-experience-of-antibiotic-use-in-pts-over-65-13-2048.jpg)