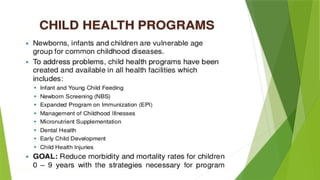
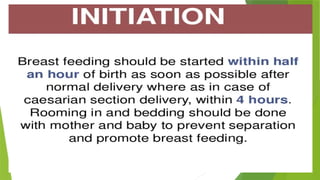
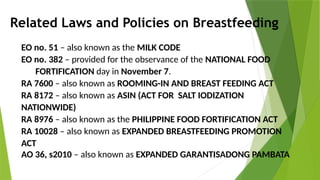
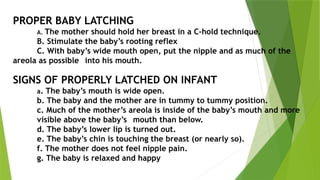
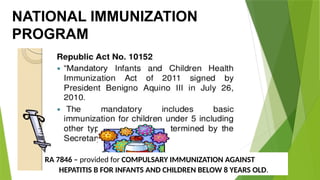
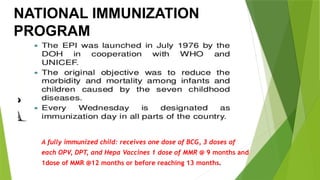
The document outlines essential practices and policies surrounding breastfeeding, newborn care, immunization, and nutrition in the Philippines. It covers the benefits of breastfeeding, guidelines for complementary feeding, and the significance of newborn screening for metabolic disorders. It also details the national immunization program, including recommended vaccines, storage requirements, and management of potential side effects.