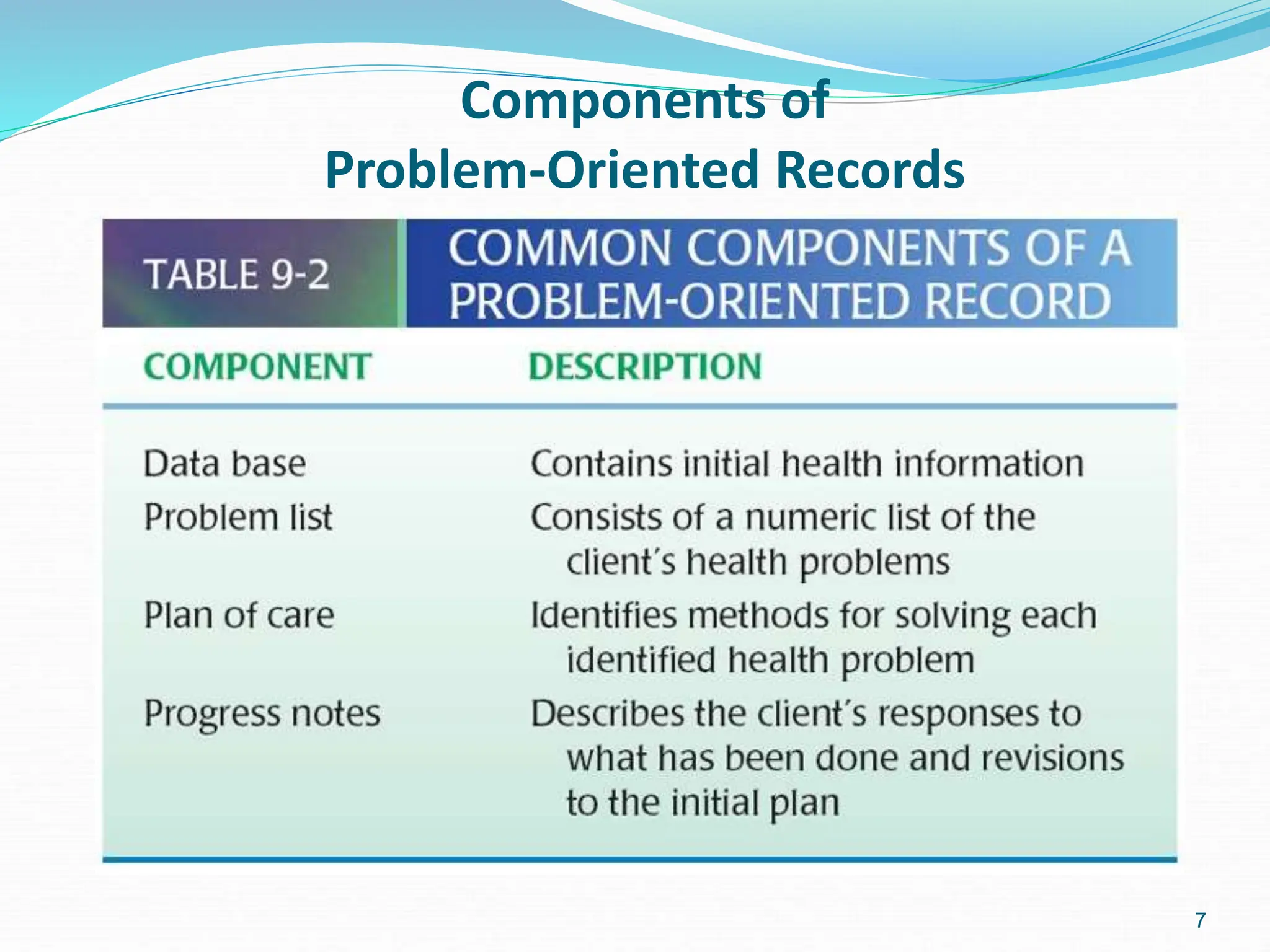
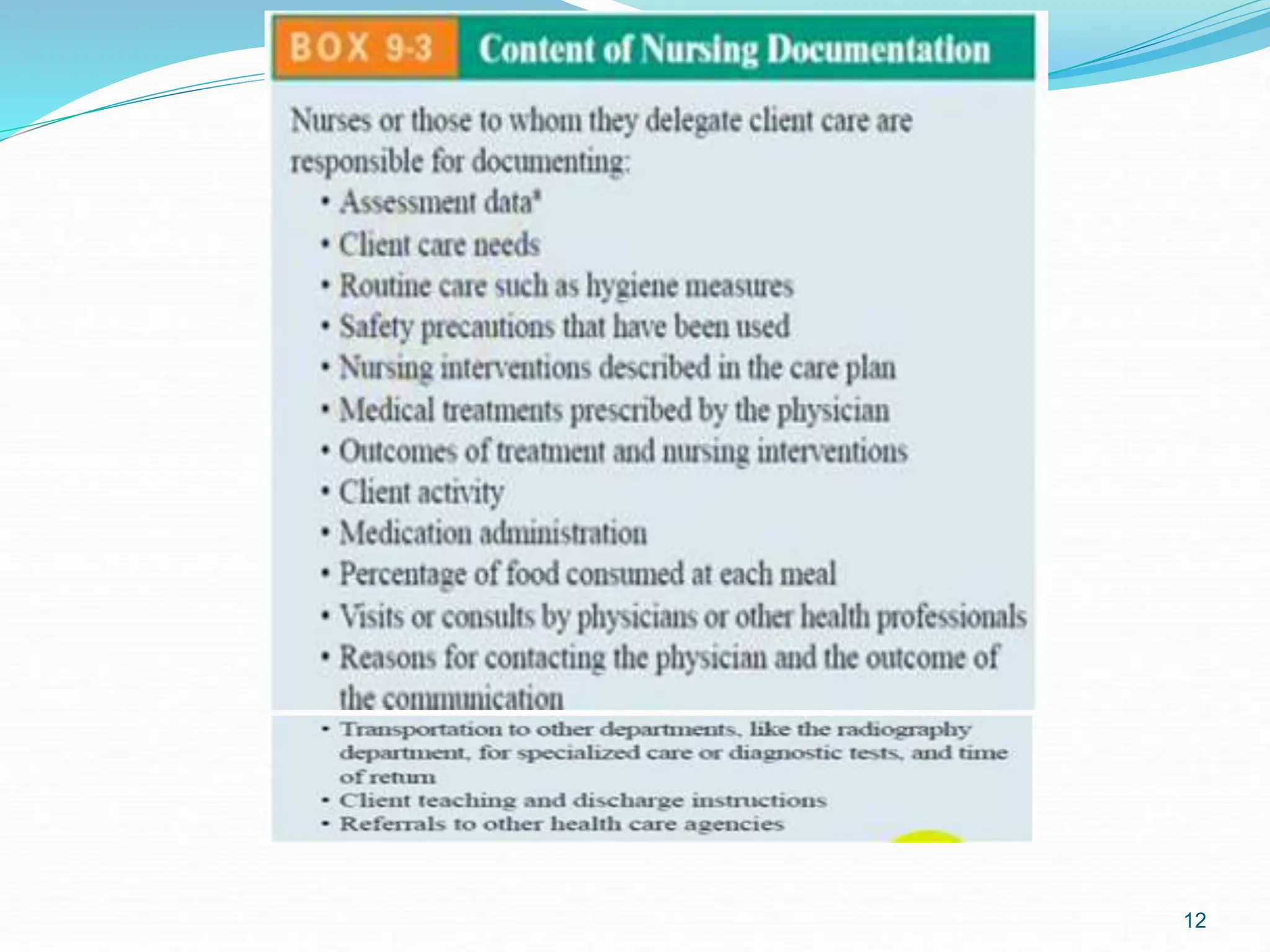
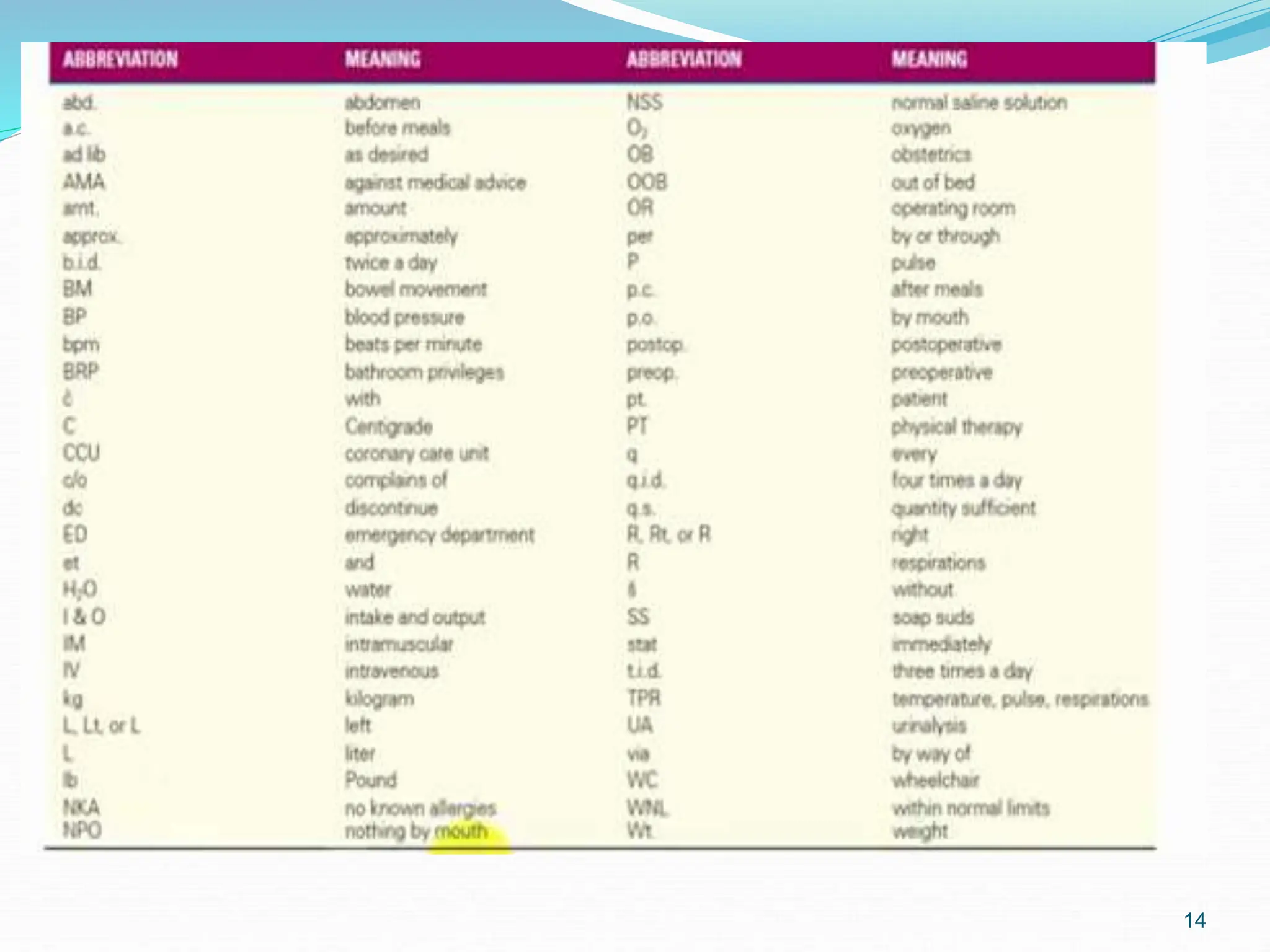
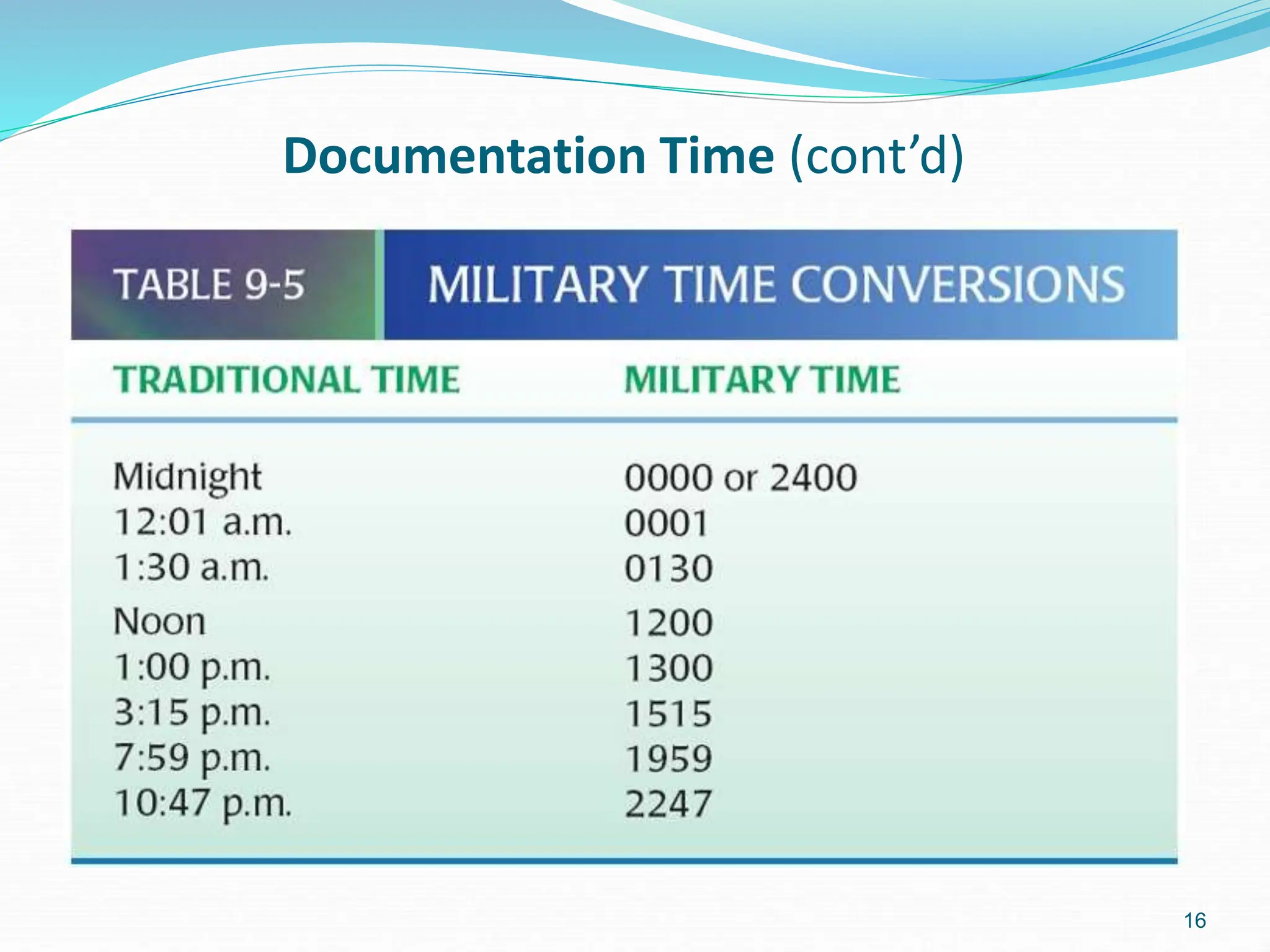
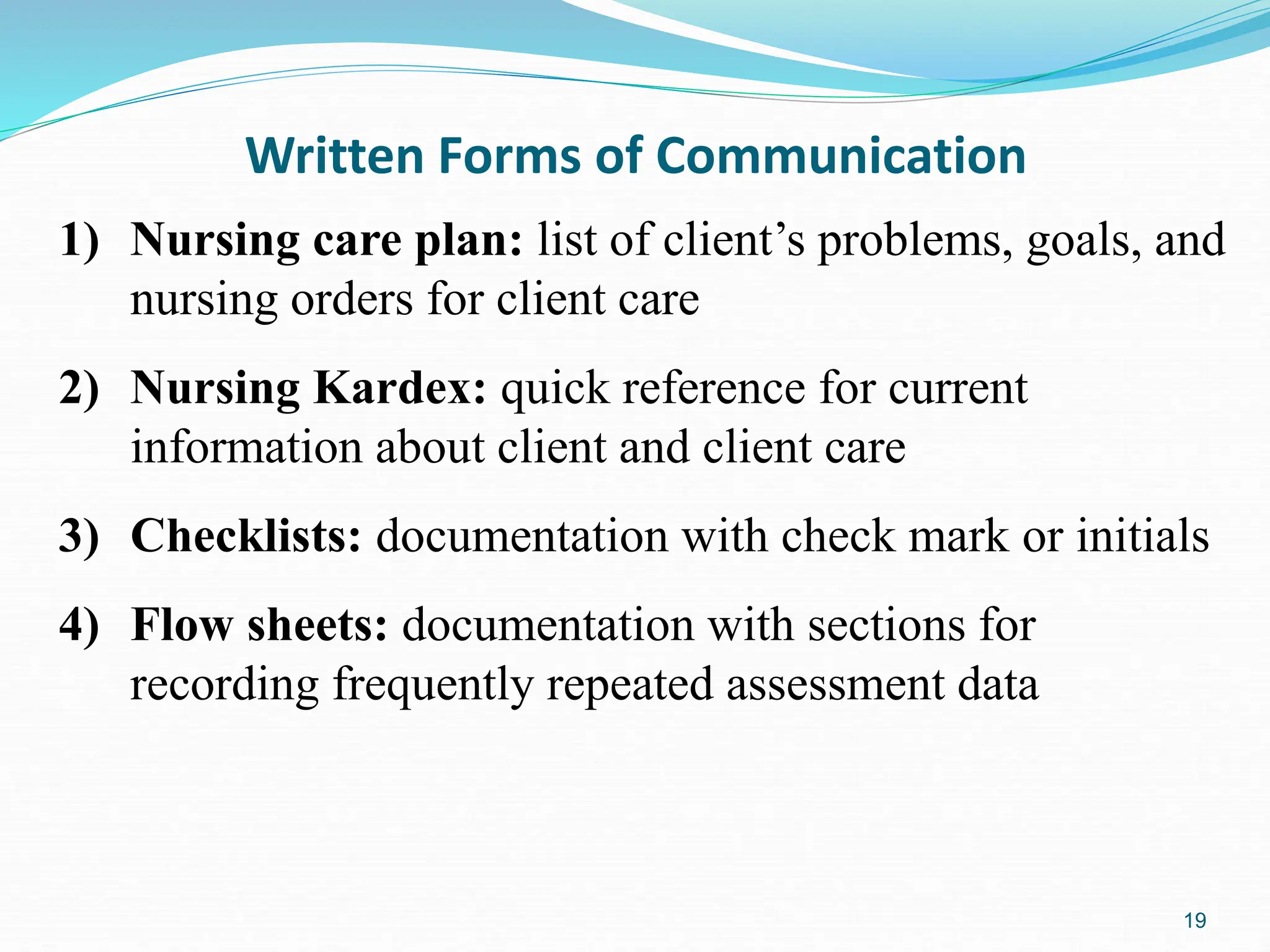
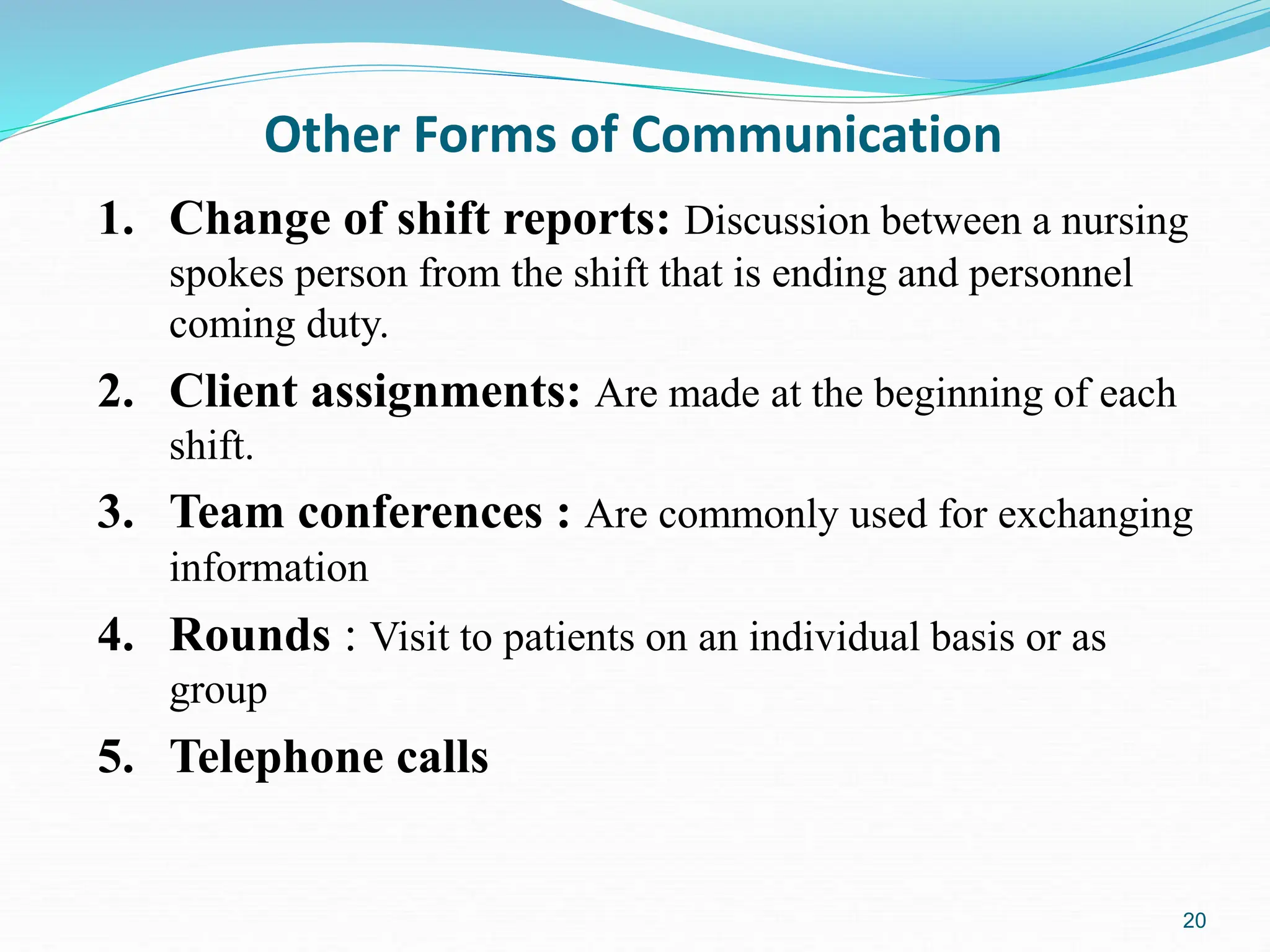
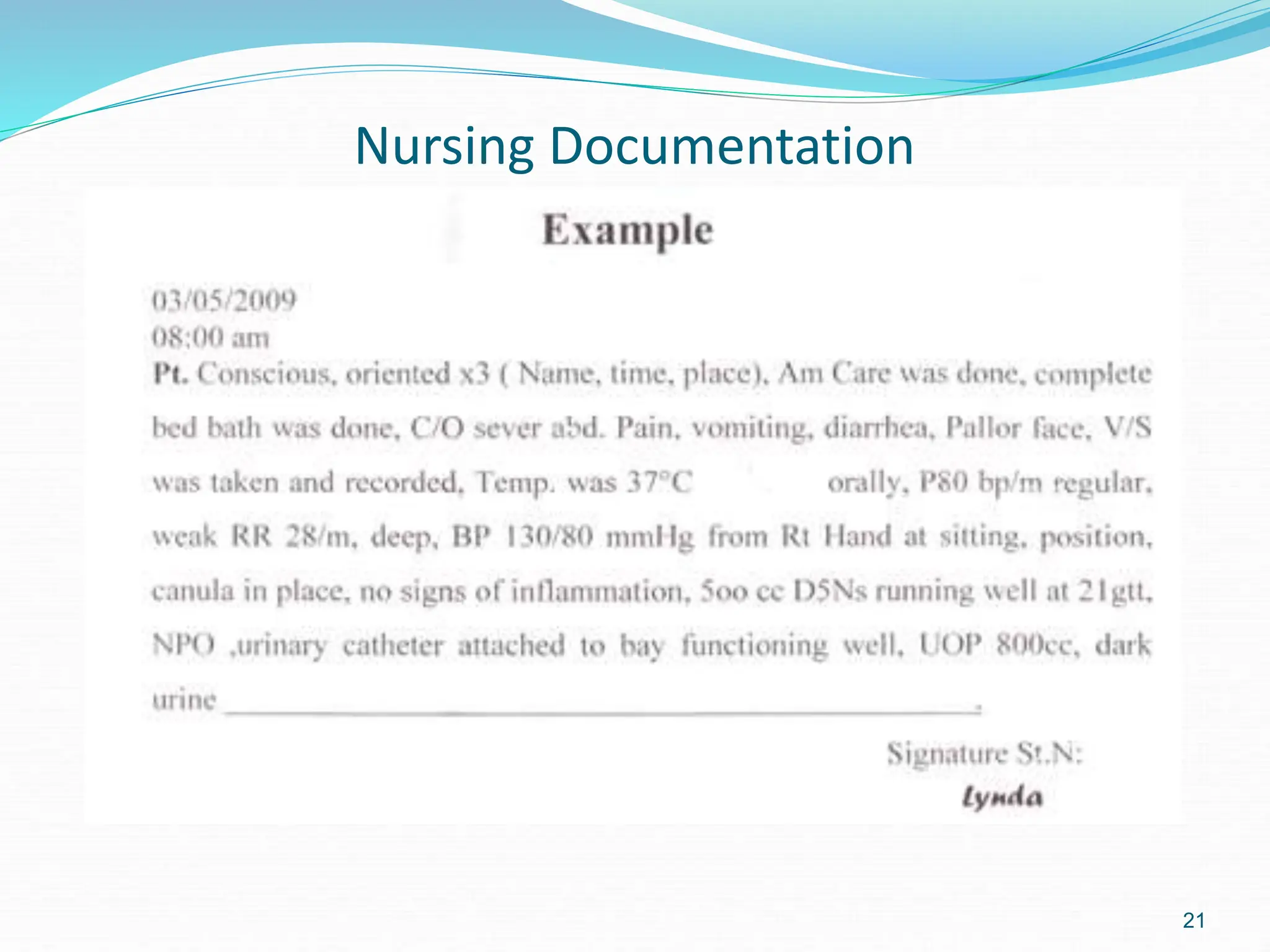
Medical records, also known as health or client records, are written collections of information about a person's health, care received, and progress. They have several uses including permanent records, sharing information between providers, quality assurance, accreditation, reimbursement, education, and legal evidence. Components include health information, care provided, progress, and care plans. Records can be organized by source or problem, and common charting methods include narrative, SOAP, and computerized documentation. Proper documentation follows guidelines for clarity, time recording, and use of approved abbreviations.