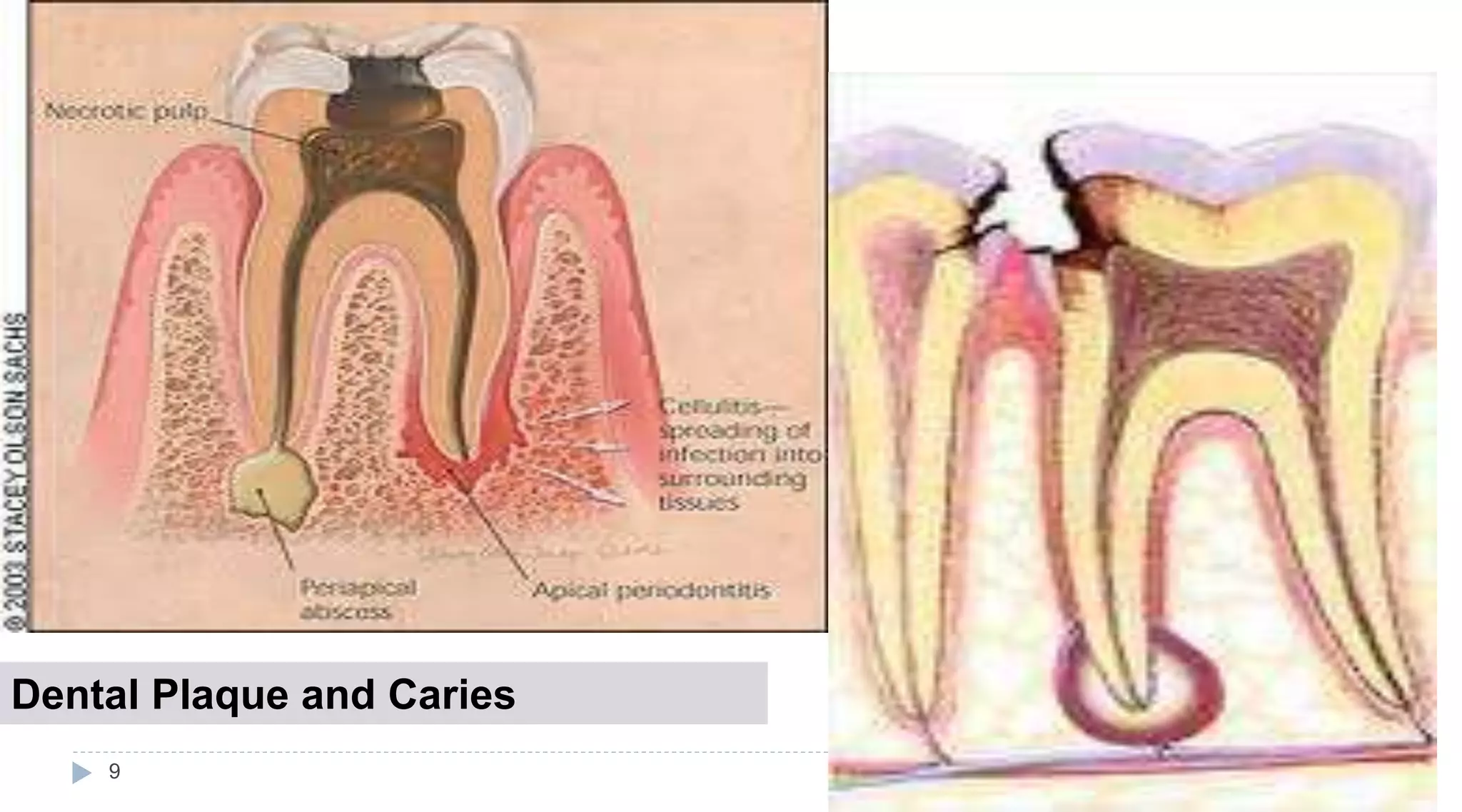
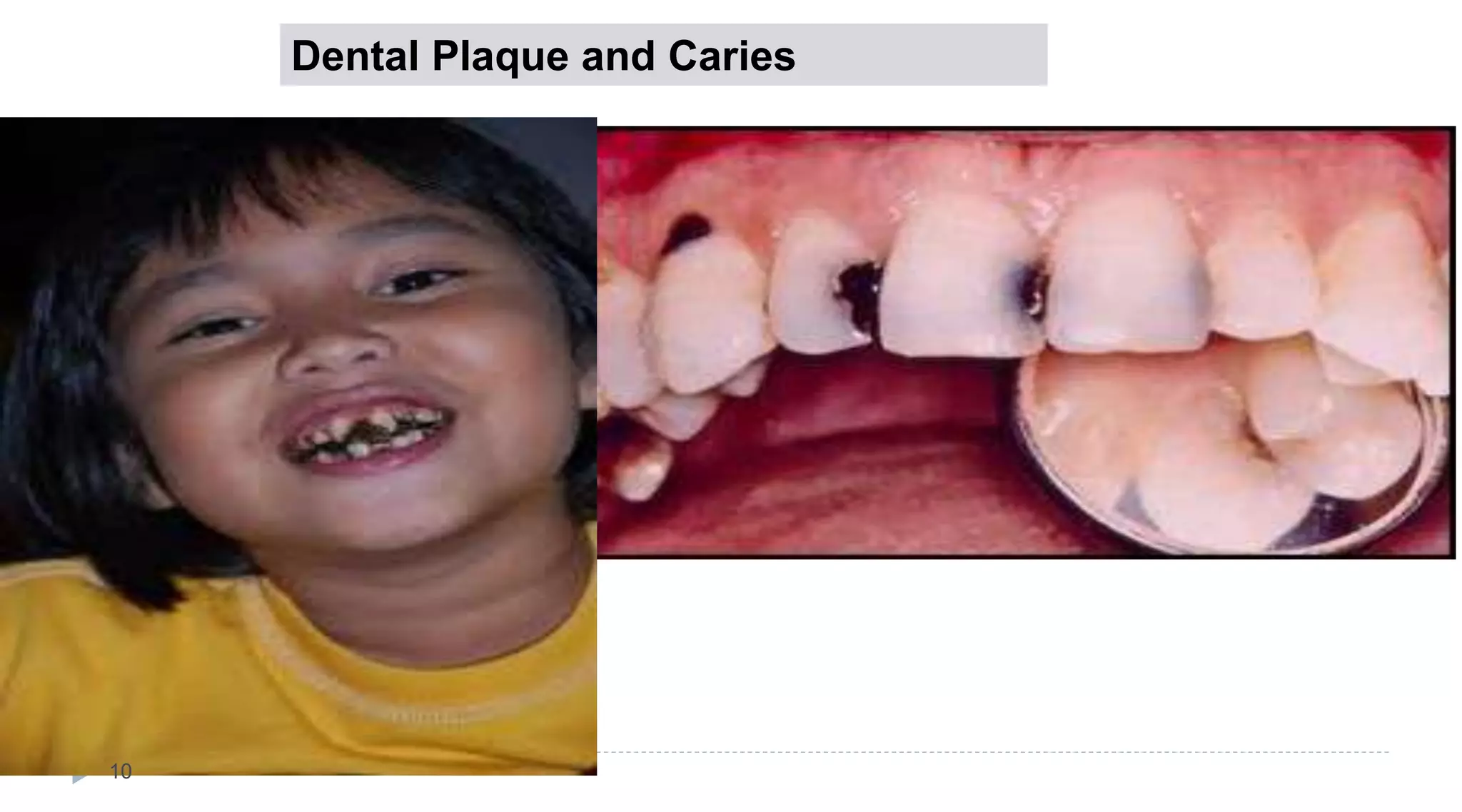
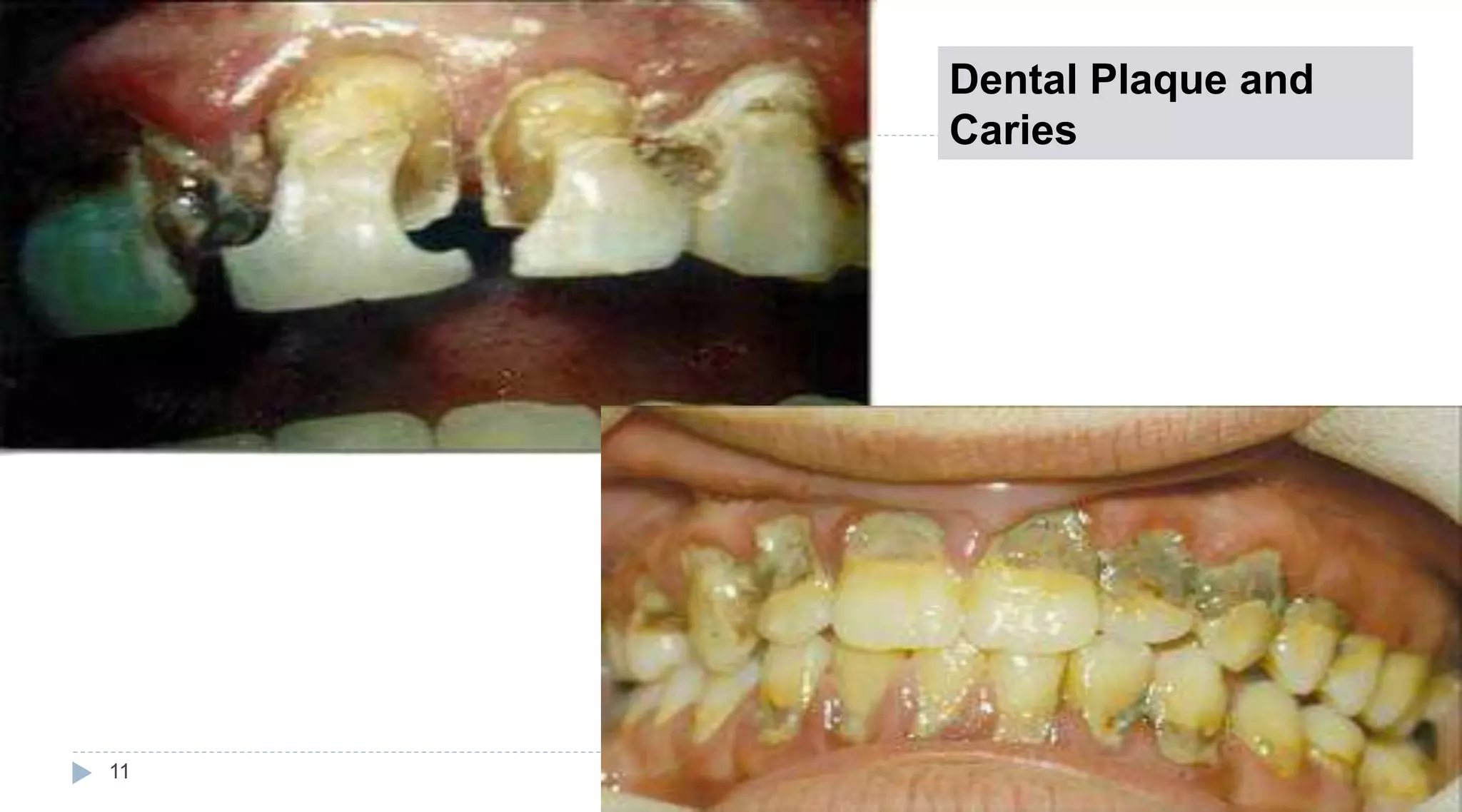
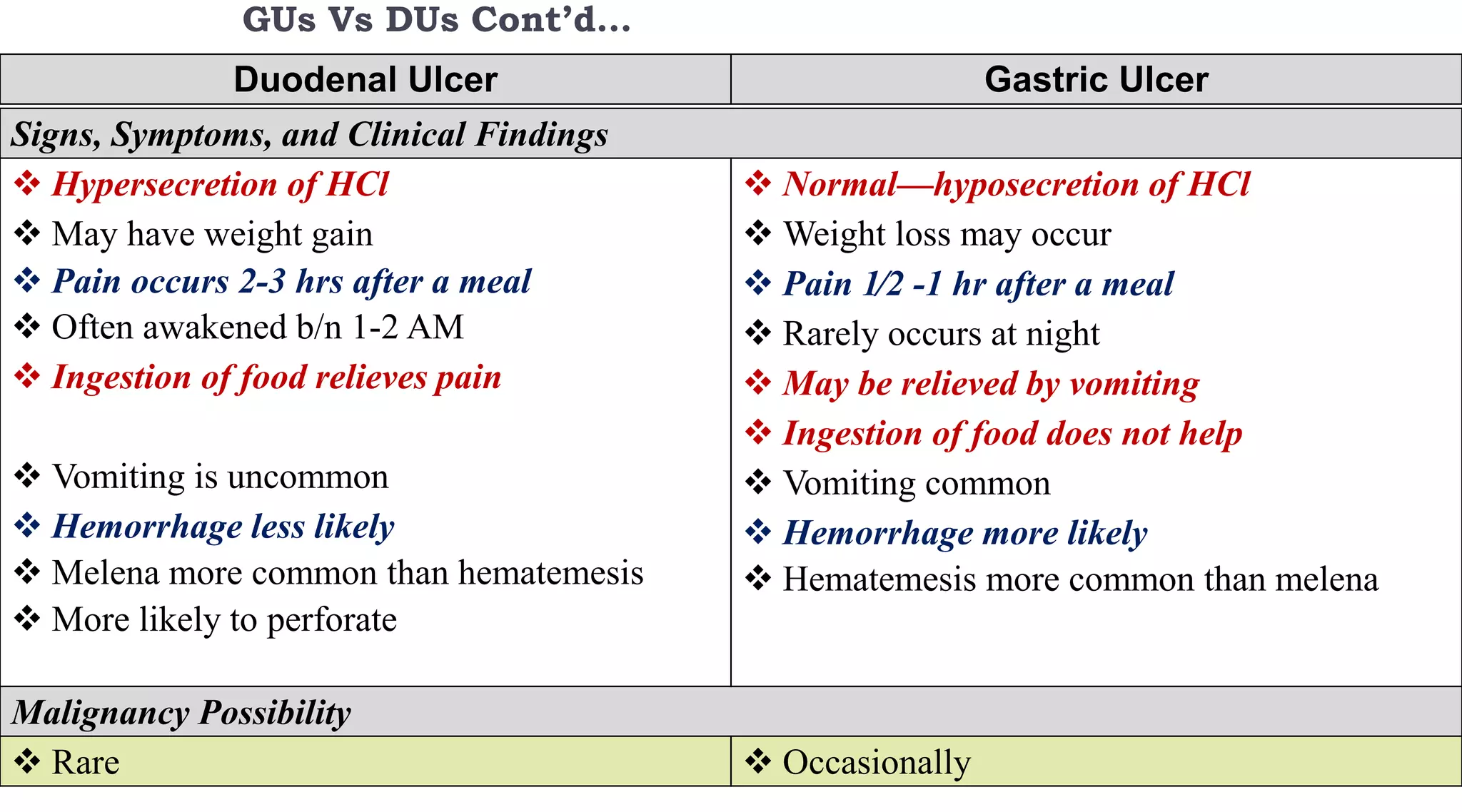
Dental plaque and caries are caused by bacteria in the mouth that metabolize sugars to produce acids. These acids demineralize tooth enamel over time, leading to cavities and damage. Proper oral hygiene through brushing, flossing, and professional cleanings can help remove plaque and prevent caries. Dietary choices like limiting sugar intake and drinking fluoridated water also reduce risk. Left untreated, caries can progress to pulpitis, abscesses, or tooth loss. Gingivitis is a mild form of gum inflammation due to plaque that can be reversed, while periodontitis involves deeper infection and bone loss requiring treatment to stop progression.


![STAGES OF GINGIVITIS
20
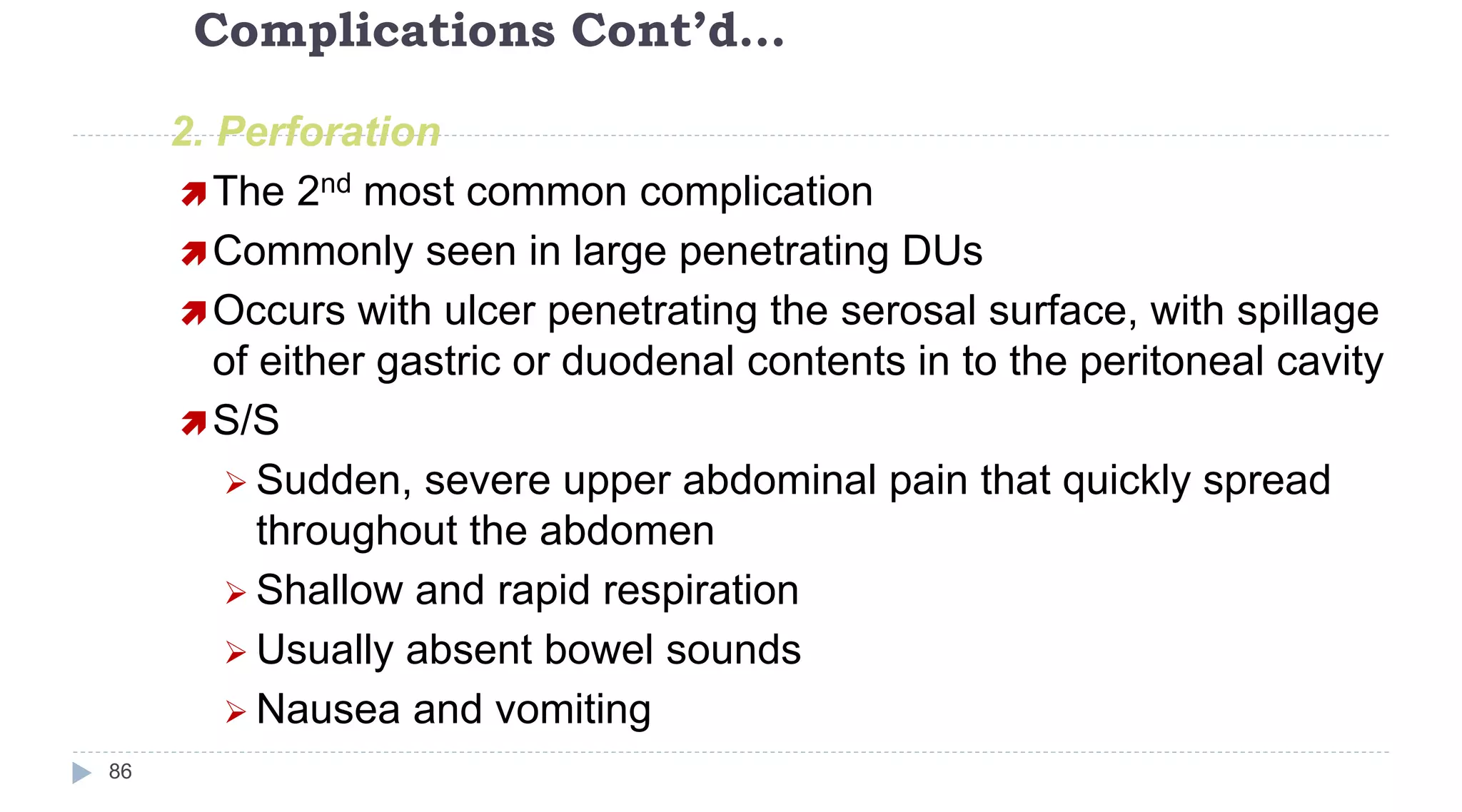
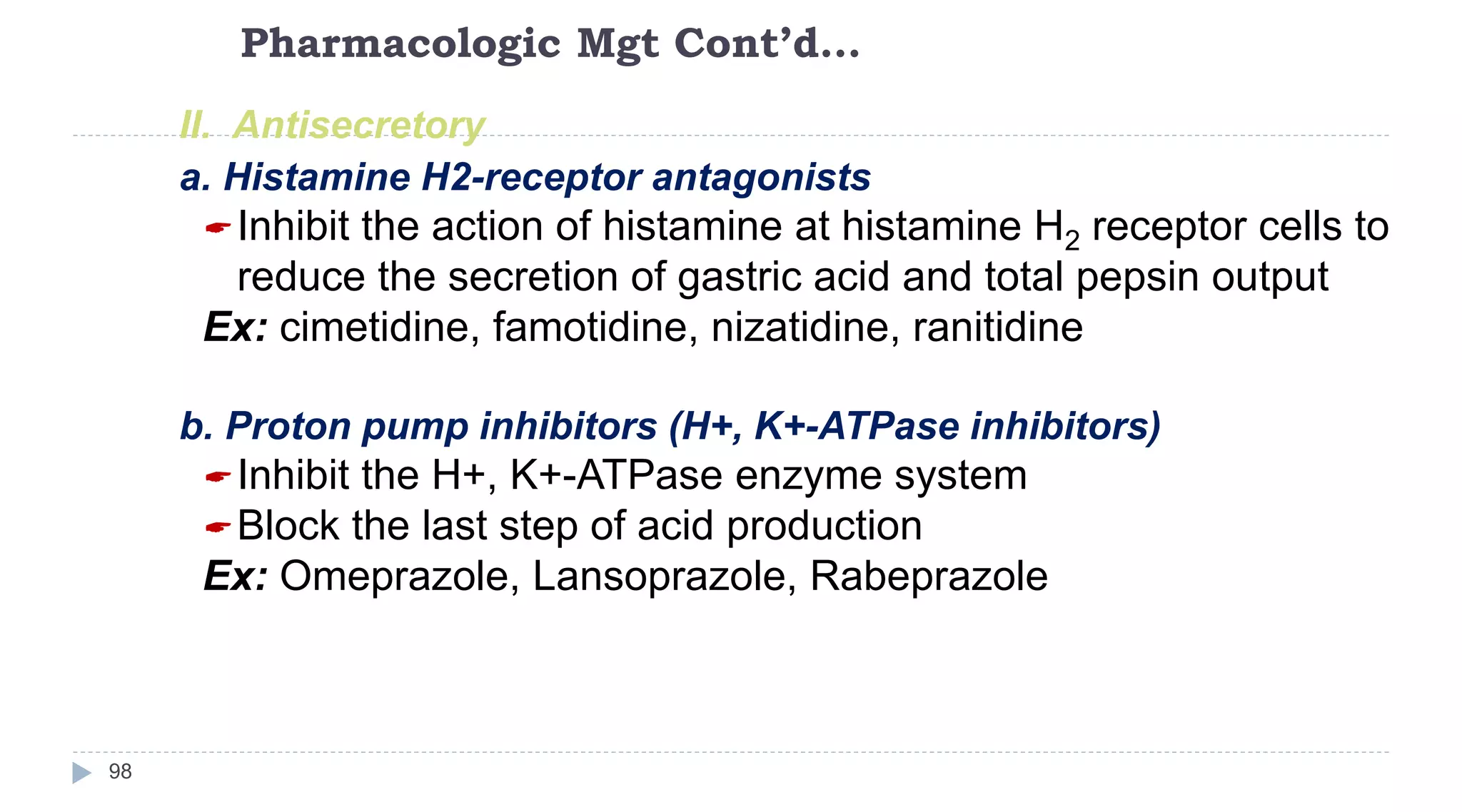
STAGE I : THE INITIAL LESION(2-4 days)
Vascular changes dilated capillaries and increased
blood flow.
Initial inflammatory changes due to microbial activation
of resident leukocytes and stimulation of endothelial
cells.
STAGE II : THE EARLY LESION
Clinical signs : ERYTHEMA[proliferation of capillaries and increased
formation of capillary loops between rete pegs].
• Evidence of bleeding on probing.
• Increase in gingival fluid flow and number of trans migrating
leukocytes[also T lymphocytes].
• Amount of collagen destruction increases which is related to Matrix
Metalloproteins
](https://image.slidesharecdn.com/disordersofuppergitsystemppt3-221229123241-3f322038/75/Disorders-of-Upper-GIT-system-ppt-3-ppt-20-2048.jpg)
.
Lesion is moderately to severely inflamed
STAGE IV : THE ADVANCED LESION
Extension of the lesion into the alveolar bone.
Phase of periodontal breakdown[bone loss].
All types of inflammatory cells.](https://image.slidesharecdn.com/disordersofuppergitsystemppt3-221229123241-3f322038/75/Disorders-of-Upper-GIT-system-ppt-3-ppt-21-2048.jpg)
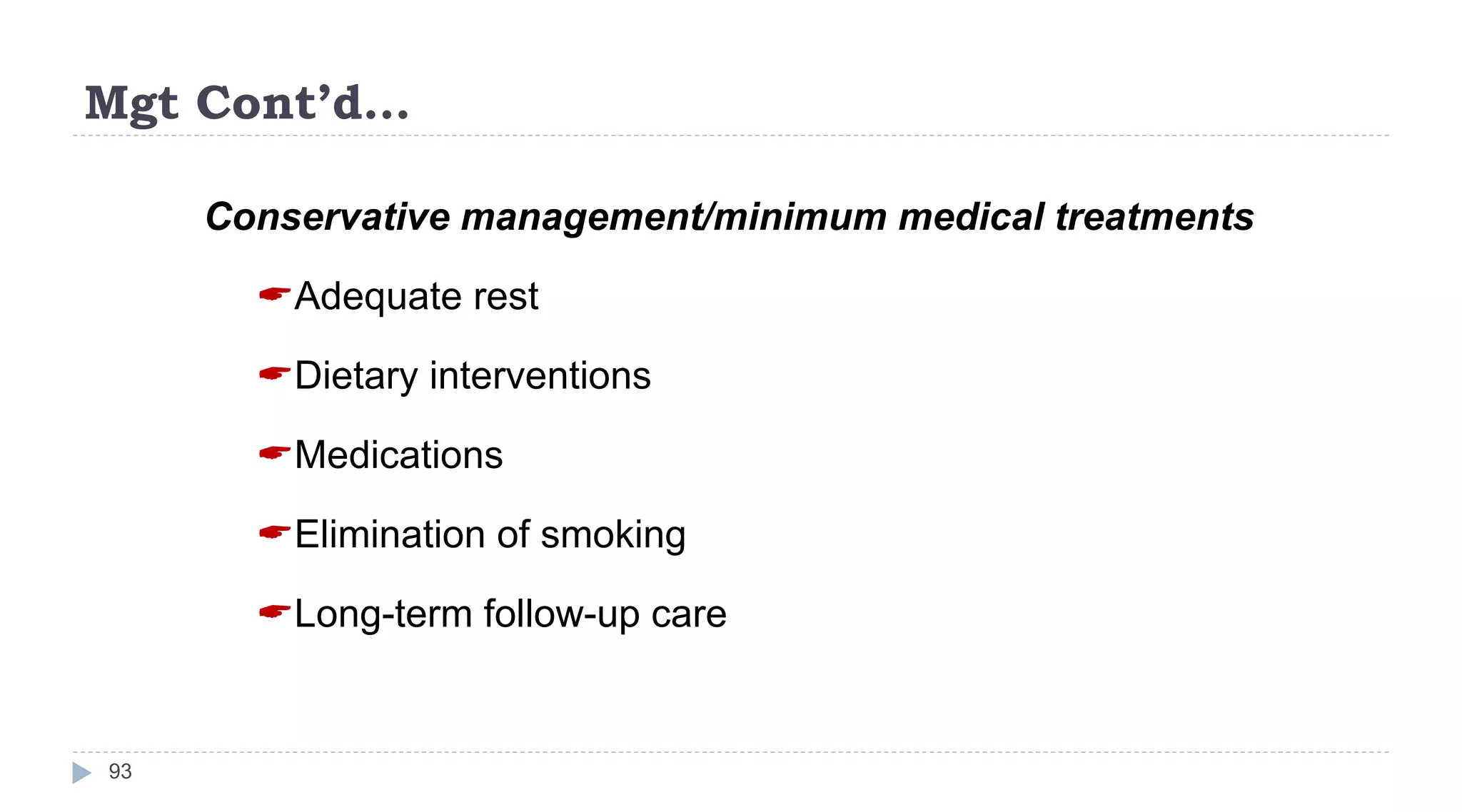






![Nursing Diagnoses may include:
225
1.Activity intolerance related to fatigue, general debility, muscle
wasting, and discomfort
2.Imbalanced nutrition, less than body requirements, related to
chronic gastritis, decreased GI motility, and anorexia
3.Impaired skin integrity related to compromised immunologic
status, edema, and poor nutrition
4.Fluid Volume excess related to compromised regulatory
mechanism (e.g., syndrome of inappropriate antidiuretic
hormone [SIADH], decreased plasma proteins, malnutrition) or
excess sodium/fluid intake evidenced by edema, anasarca,
weight gain
5.Knowledge, deficient regarding condition, prognosis, treatment,
self-care, and discharge](https://image.slidesharecdn.com/disordersofuppergitsystemppt3-221229123241-3f322038/75/Disorders-of-Upper-GIT-system-ppt-3-ppt-225-2048.jpg)