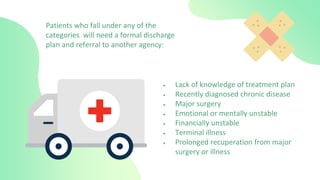
The document discusses discharge and transfer procedures in a hospital setting. It defines discharge as when patients are released from the hospital after treatment and no longer need in-patient care. It also discusses the importance of discharge planning and educating patients and caregivers on home care needs. Transfer involves moving patients within or between facilities, which requires coordination and communication between medical teams. Key aspects of discharge and transfer include assessing patient needs, educating families, and ensuring continuity of care during transitions.