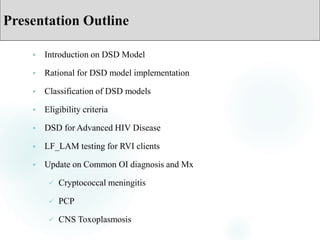
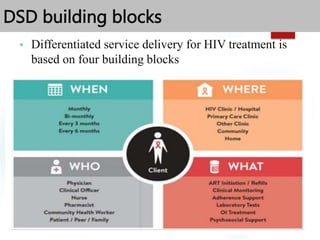
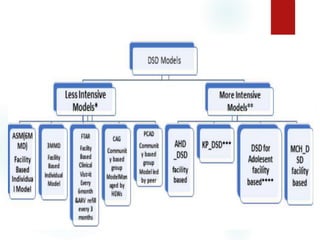
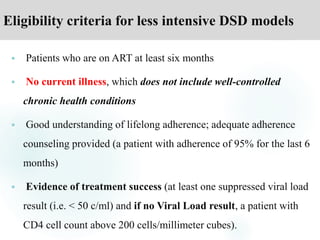
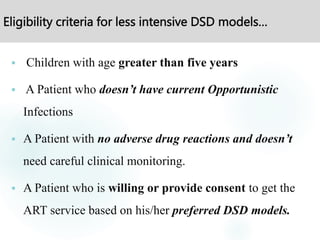
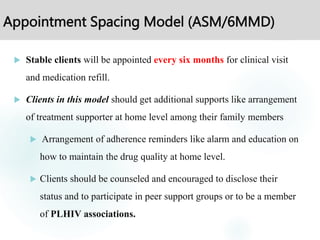
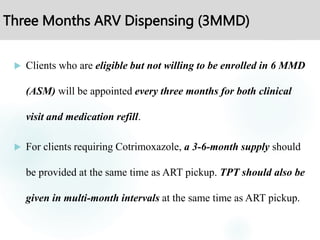
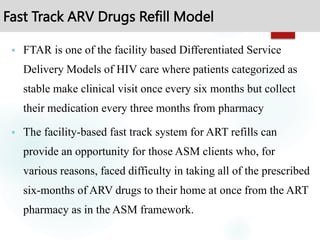
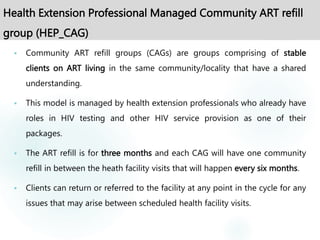
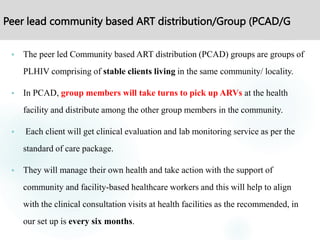
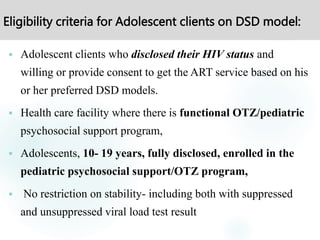
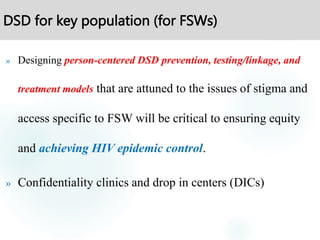
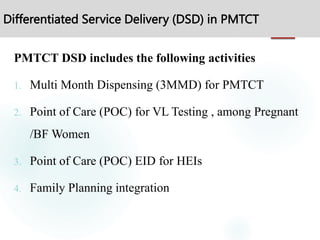
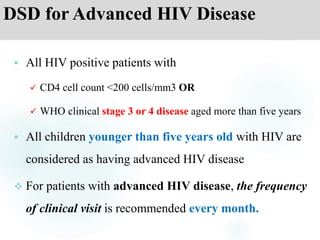
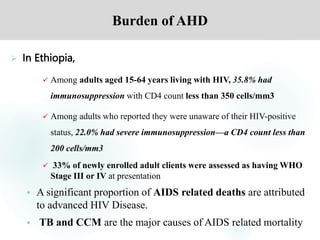
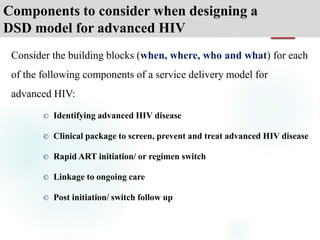
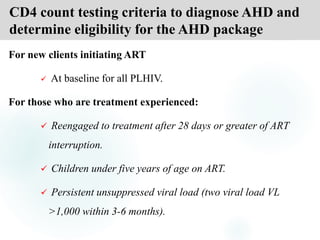
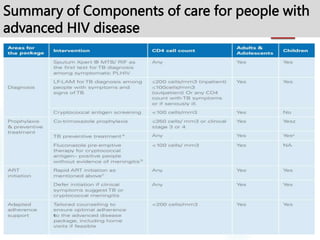
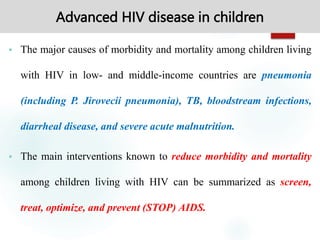
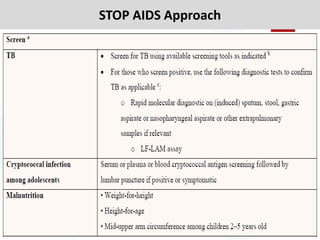
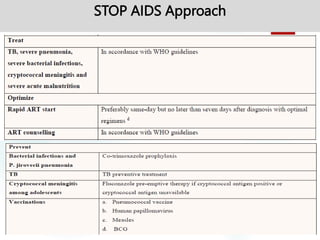
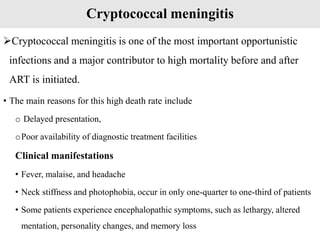
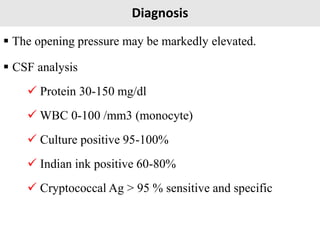
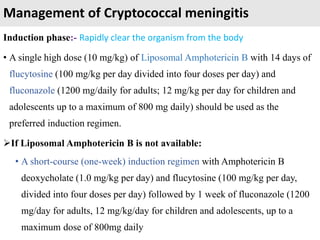
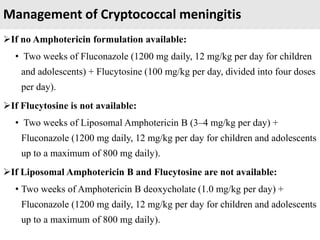
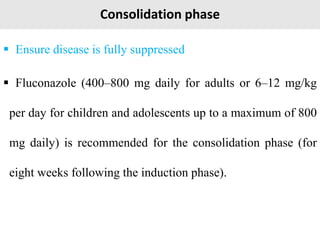
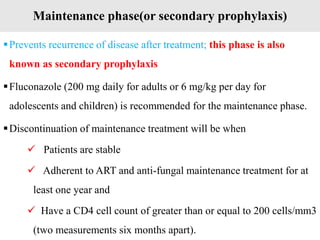
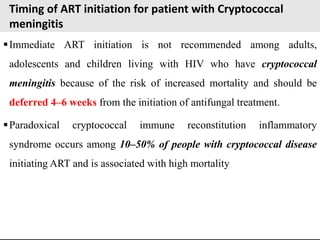
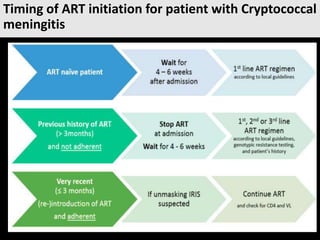
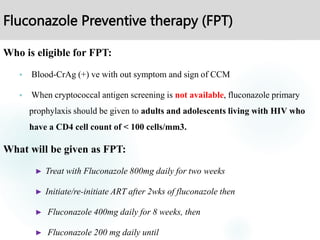
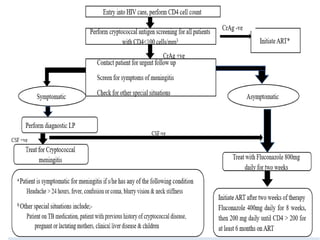
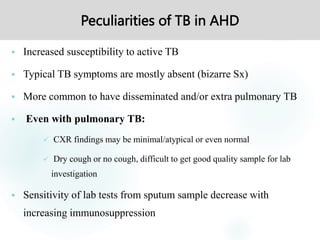
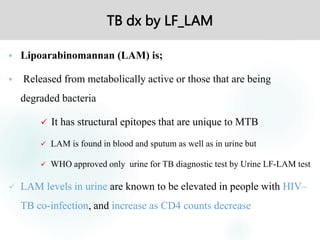
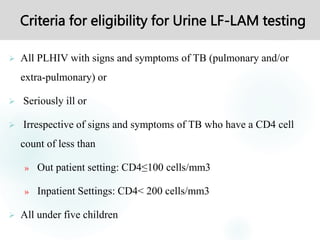
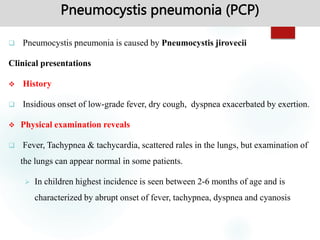
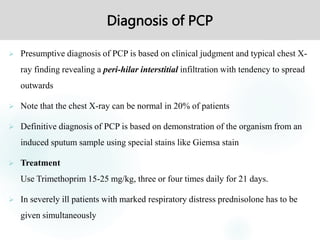
The document outlines the Differentiated Service Delivery (DSD) model for advanced HIV disease, emphasizing a client-centered approach to tailoring HIV services for various patient needs. It discusses criteria for different DSD models, which include less intense options for stable patients and more intensive care for those with complications, such as opportunistic infections. Additionally, the document addresses advanced HIV disease management, including treatment protocols for opportunistic infections like cryptococcal meningitis and guidelines for monthly clinical visits for affected patients.