Embed presentation
Downloaded 100 times


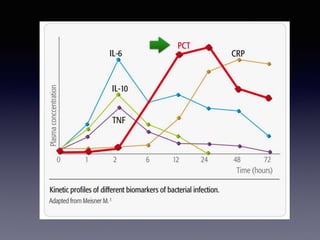

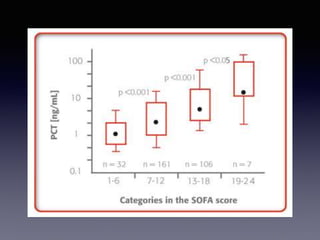

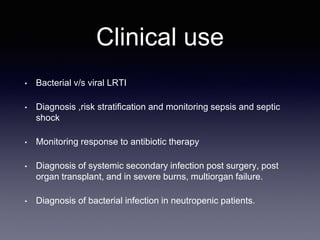
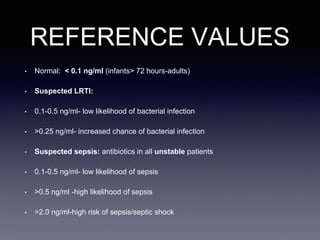







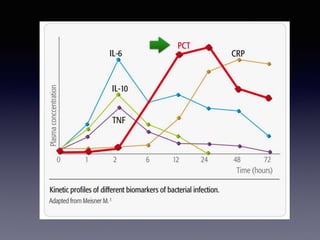
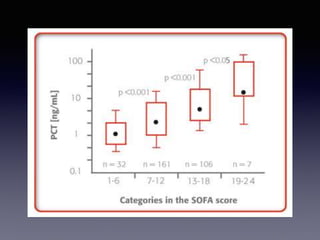
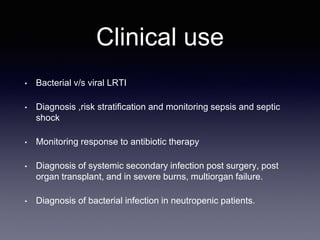
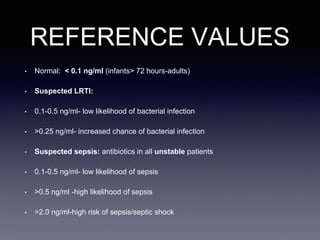
Procalcitonin is a biomarker that is more specific than others for bacterial infection. It rises rapidly within 6 hours of an insult and declines quickly with treatment. It is not impacted by anti-inflammatory states and correlates well with illness severity. Procalcitonin levels can be used to differentiate between bacterial and viral lung infections, diagnose and monitor sepsis and septic shock, monitor antibiotic treatment response, and diagnose secondary infections. Reference values are provided and recommendations include measuring PCT at initiation of suspected conditions and repeating every 2-3 days to guide antibiotic use along with culture and clinical data.