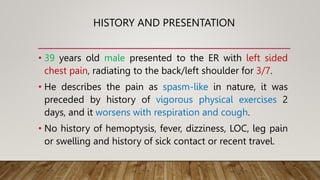
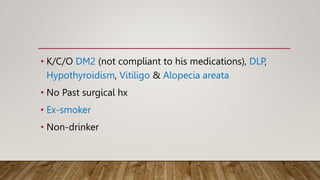
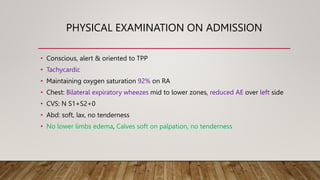
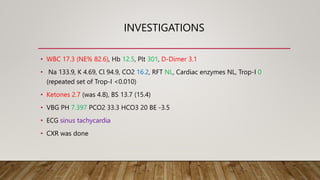
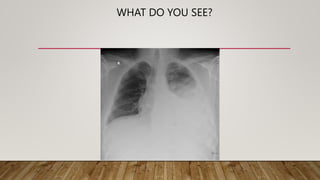
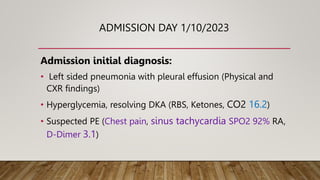
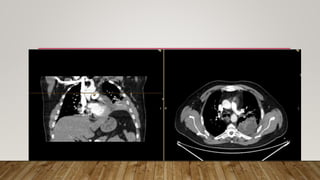
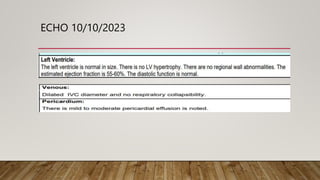
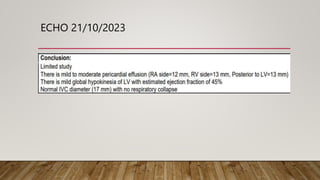
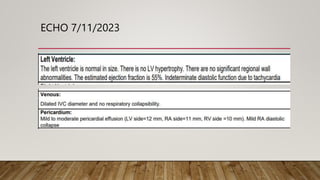
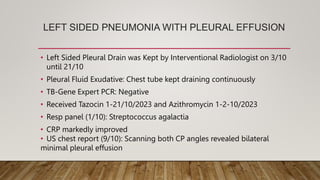
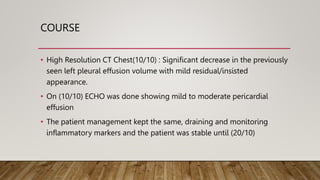
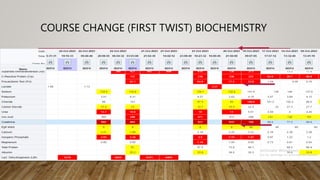
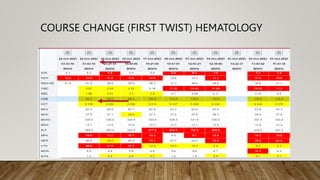
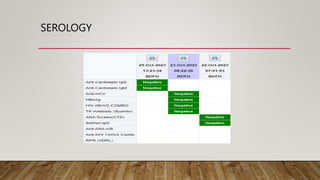
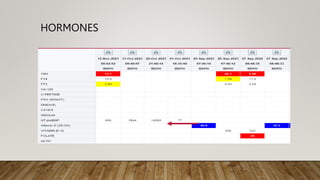
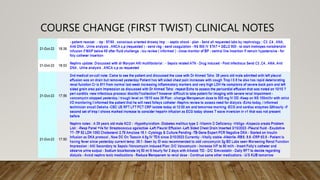
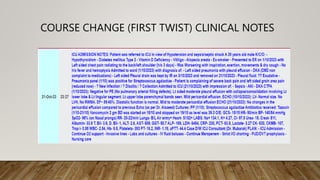
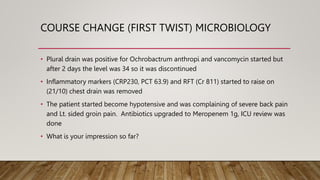
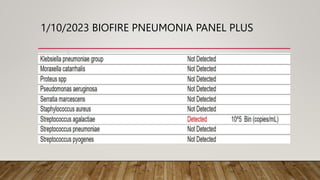
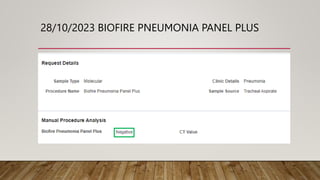
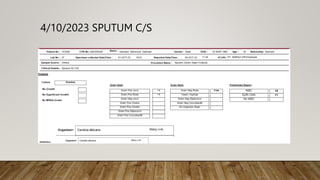
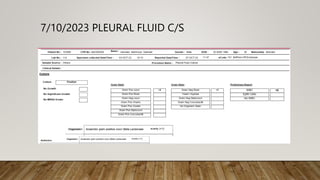
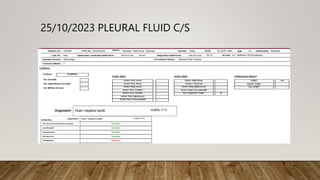
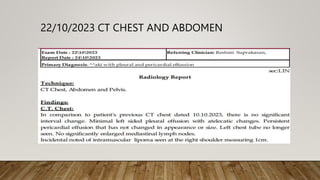
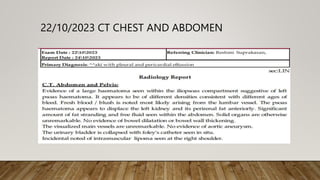
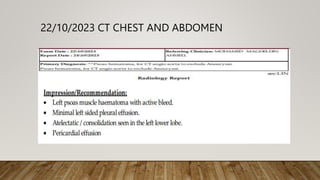
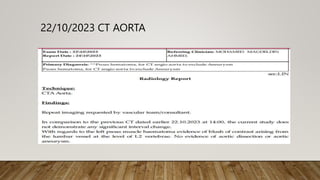
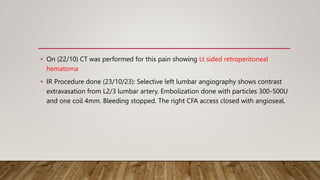
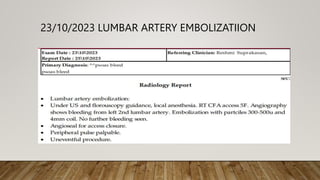
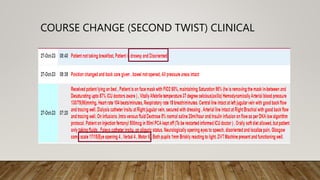
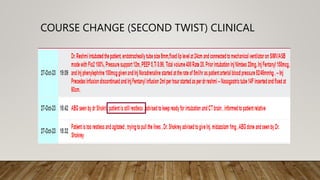
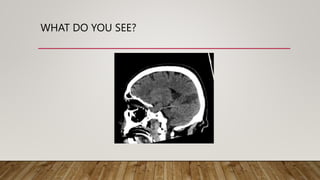
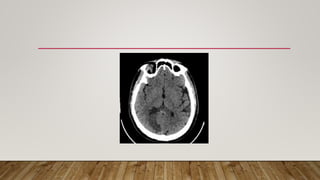
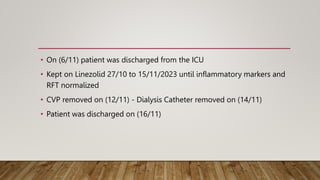
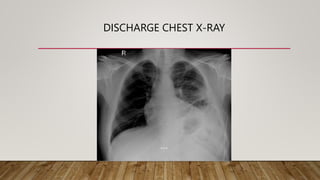
A 39-year-old male presented with left-sided chest pain and was diagnosed with left-sided pneumonia and pleural effusion, as well as hyperglycemia and suspected pulmonary embolism. He underwent various tests and treatments, including a pleural drain, antibiotics, and an interventional radiology procedure for a retroperitoneal hematoma. The patient was stabilized and discharged after treatment for ongoing infections and normalized inflammatory markers.