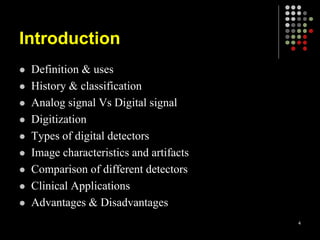
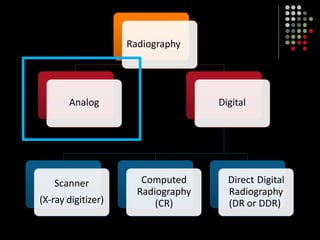
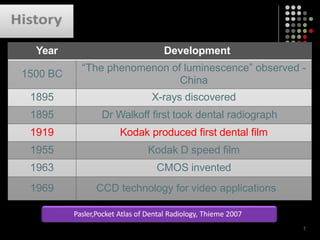
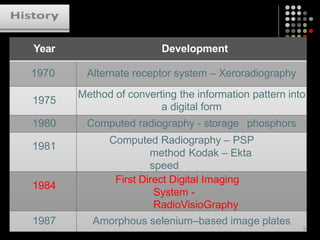
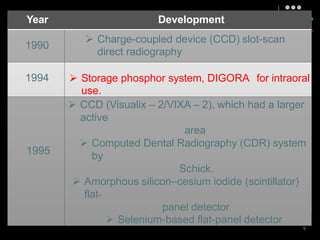
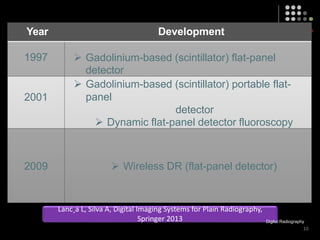
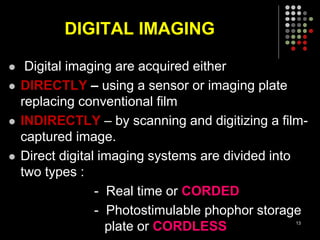
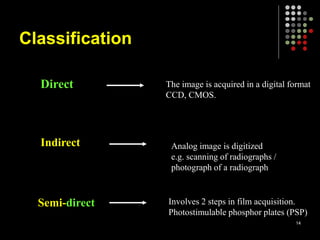
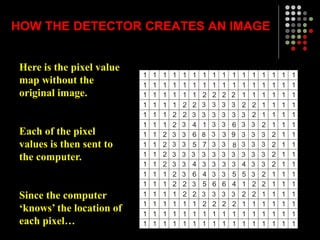
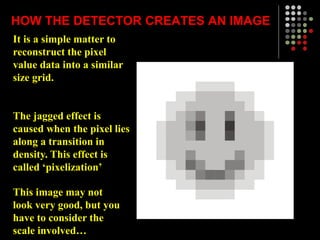
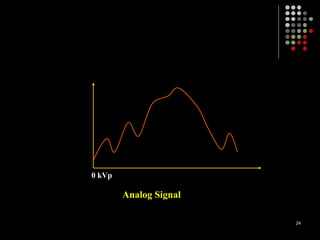
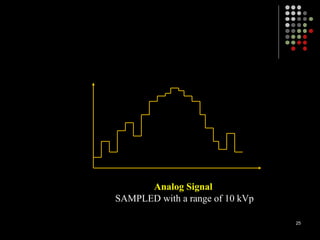
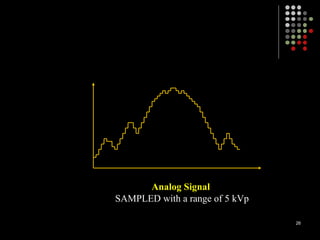
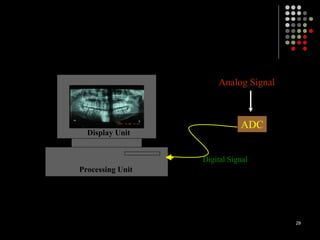
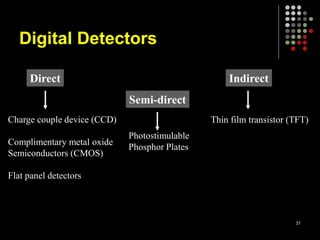
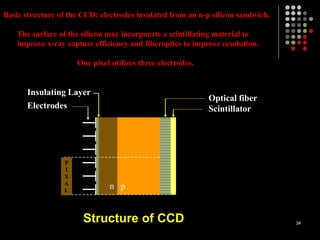
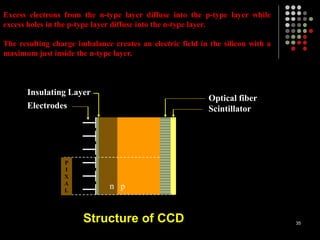
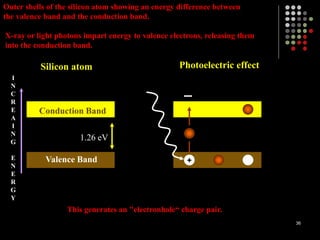
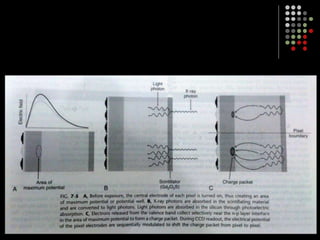
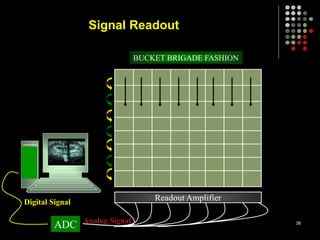
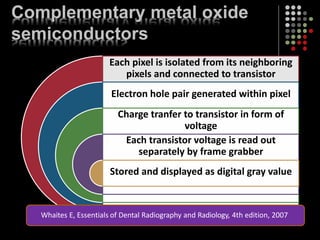
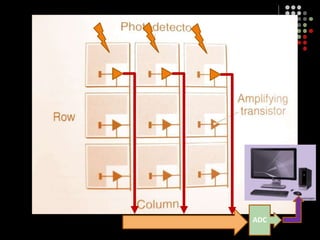
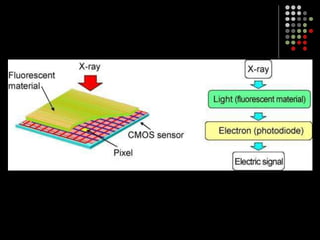
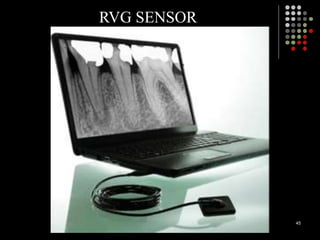
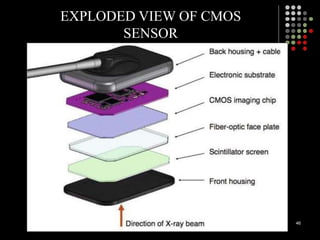
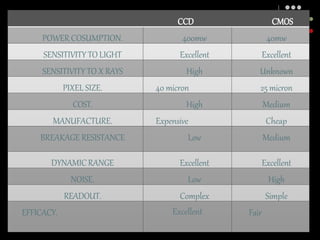
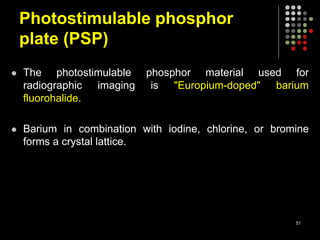
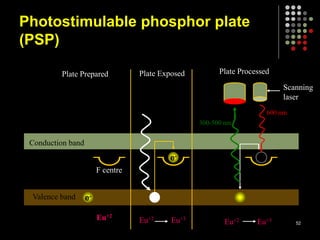
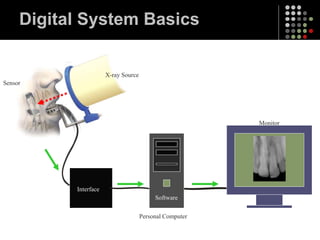
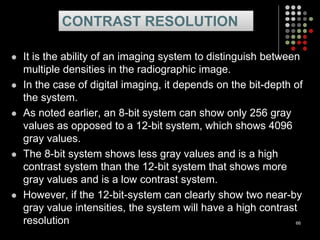
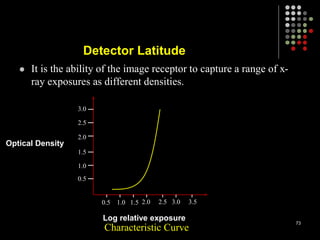
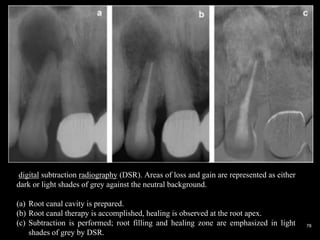
The document provides an overview of digital imaging in dentistry, discussing its definition, historical development, and various methods and technologies. Key topics include the comparison of digital detectors, analog versus digital signals, and clinical applications alongside their advantages and disadvantages. Further details are provided on imaging techniques such as direct and indirect digital imaging, the structure of charge-coupled devices (CCDs) and complementary metal oxide semiconductors (CMOS), and the implications for dental radiography.