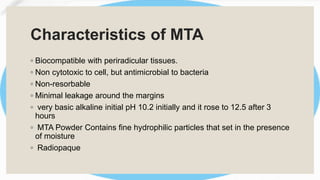
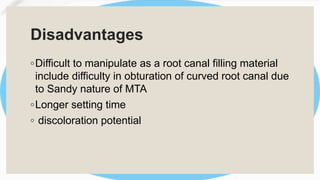
The document provides an overview of various types of dental cements, including glass ionomer cements, resin cements, and mineral trioxide aggregate cement, highlighting their compositions, properties, and clinical applications. Key points include the advantages and limitations of each cement type, such as biocompatibility, bonding strength, and setting reactions. It concludes that no single cement type meets all ideal requirements, emphasizing the importance of selecting appropriate materials based on clinical situations.