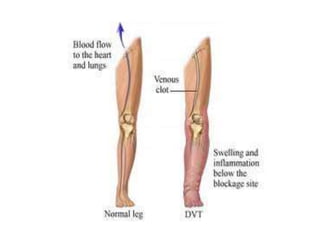
A venous thrombus is a blood clot that forms in the veins. It can lead to a pulmonary embolism if parts of the clot break off and travel to the lungs. Venous thrombosis is caused by damage to the vessel wall, slowed blood flow, and increased coagulability. Risk factors include injuries to the lower limbs, pregnancy, oral contraceptives, and cancer. Diagnosis involves testing for d-dimer and ultrasound imaging of the veins. Treatment consists of blood thinners like heparin and warfarin to prevent clot growth as well as thrombolysis to break up existing clots.