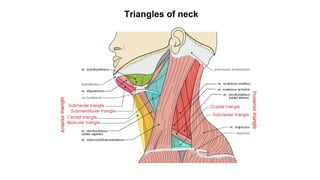
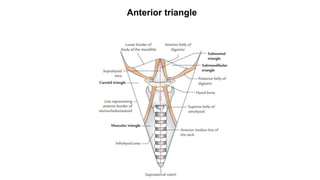
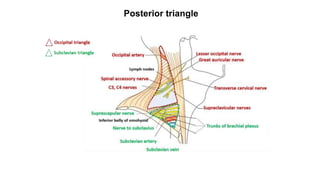
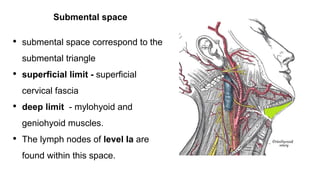
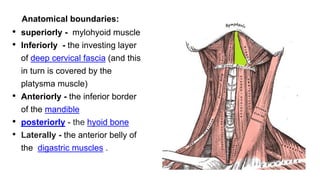
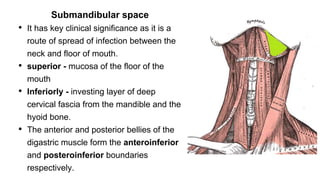
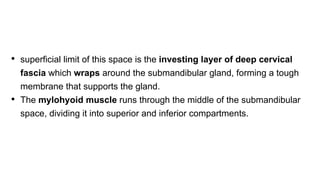
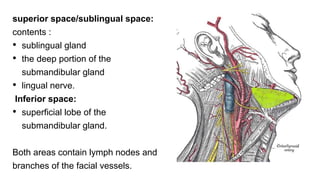
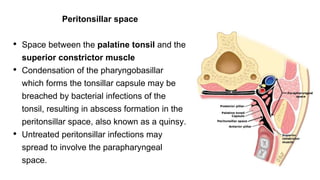
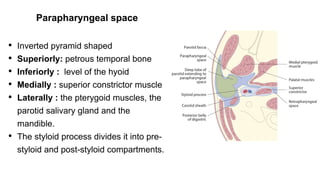
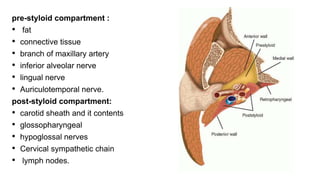
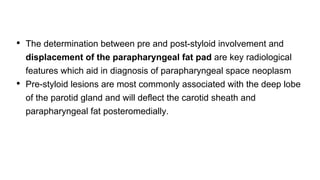
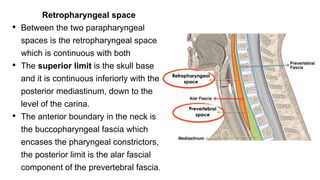
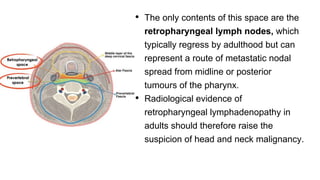
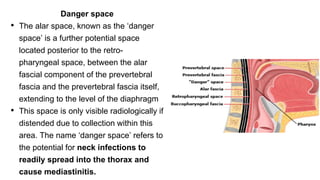
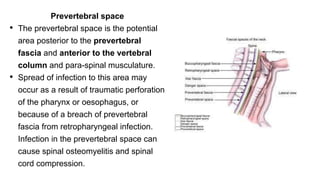
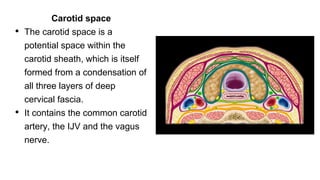
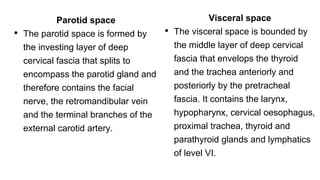
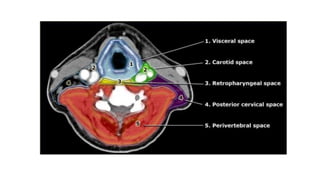
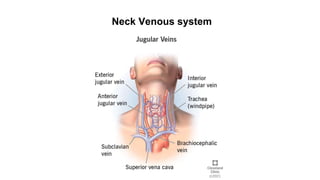
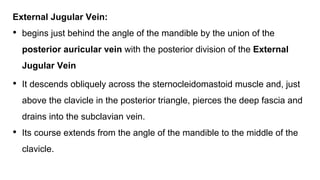
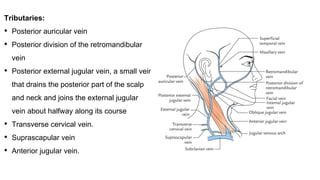
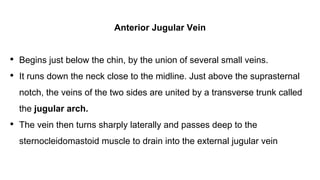
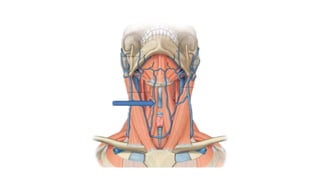
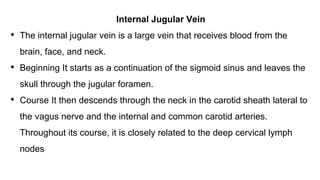
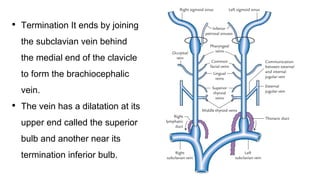
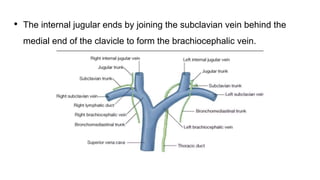
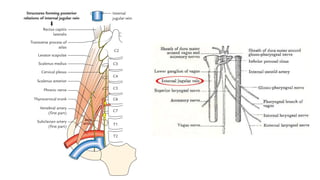
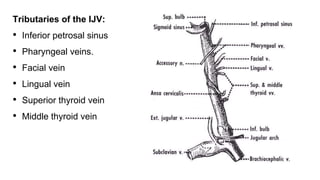
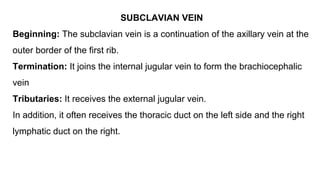
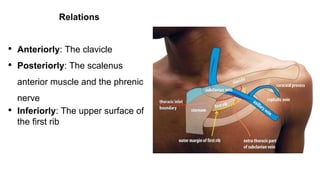
This document summarizes several anatomical spaces in the neck, including the submental, submandibular, peritonsillar, parapharyngeal, retropharyngeal, prevertebral, carotid, parotid, and visceral spaces. It also describes key structures and contents of each space. Additionally, it reviews the neck venous system, describing veins such as the external jugular, anterior jugular, internal jugular, subclavian, and their tributaries. The document provides clinical relevance for several spaces as routes of infection spread.