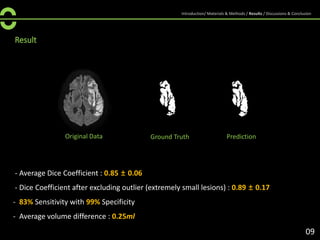
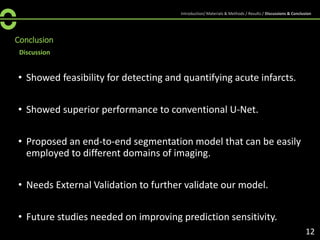
The document discusses a deep learning-based automated model for detecting and quantifying acute infarcts in ischemic stroke using diffusion-weighted imaging (DWI). The proposed modified 3D U-Net model demonstrates superior performance in lesion detection compared to conventional methods, achieving an average Dice coefficient of 0.85 and high sensitivity and specificity rates. However, the study emphasizes the need for external validation and improvements in prediction sensitivity.

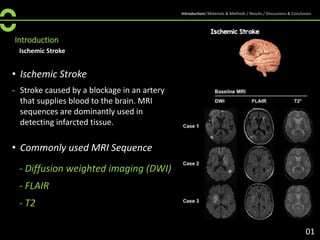
![Introduction
Imaging
• DWI MR
- DWI (a combination of T2 and diffusion
weighting) is commonly used for evaluation
of “acute ischemic stroke” for its sensitivity
in the detection of small and early infarcts
• Apparent Diffusion Coefficient Map
(ADC map)
- ADC values can be used as reference data
in acute ischemic stroke populations.
However, its reliability is continuously
questioned [1] .
[1] Fiehler, Jens, et al. "Severe ADC decreases do not predict irreversible tissue damage in humans." Stroke 33.1 (2002): 79-86.
[1]
02
Introduction/ Materials & Methods / Results / Discussions & Conclusion](https://image.slidesharecdn.com/strokersna1-201025173754/85/Deep-Learning-based-Fully-Automated-Detection-and-Quantification-of-Acute-Infarcts-4-320.jpg)
![Introduction
Deep Learning
• Deep learning approaches
- U-shaped architecture consisted of
encoder and decoder [2] is dominant in
deep learning models for detecting
ischemic stroke lesions.
- One of the main issues of deep-learning
based detection algorithms are highly
unbalanced class extent, small size of lesion,
overfitting to the train set, and lack of
annotated datasets [3].
[2] Ronneberger, Olaf, Philipp Fischer, and Thomas Brox. "U-net: Convolutional networks for biomedical image segmentation." International Conference on Medical
image computing and computer-assisted intervention. Springer, Cham, 2015.
[3] Clèrigues, Albert, et al. "Acute ischemic stroke lesion core segmentation in CT perfusion images using fully convolutional neural networks." Computers in
Biology and Medicine 115 (2019): 103487.
[2]
03
Introduction/ Materials & Methods / Results / Discussions & Conclusion](https://image.slidesharecdn.com/strokersna1-201025173754/85/Deep-Learning-based-Fully-Automated-Detection-and-Quantification-of-Acute-Infarcts-5-320.jpg)
![Introduction
• Proposal
- A deep-learning based automated infarct segmentation model on DWI was
developed.
- Infarct severity with respect to ADC map was measured.
- Deep learning algorithm is expected to detect lesion areas missed by
predictions based on ADC values.
Ensemble
Results
Prediction ADC mapping
Large lesion
Small lesion
Modified U-Net
[An overview of proposed method]
04
Proposed Method
Introduction/ Materials & Methods / Results / Discussions & Conclusion](https://image.slidesharecdn.com/strokersna1-201025173754/85/Deep-Learning-based-Fully-Automated-Detection-and-Quantification-of-Acute-Infarcts-6-320.jpg)
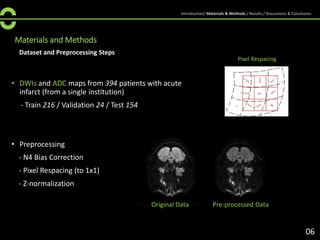
![Materials and Methods
Model
• Use Modified 3D U-Net [4] as our baseline model.
• Modified 3D U-Net adds additional deep supervision in the decoder by integrating
segmentation layers at different levels of the network
• Replace conventional 2D Convolution with Partial Convolution [5].
• Our model performs 2D segmentation.
Modified U-Net
[4] Isensee, Fabian, et al. "Brain tumor segmentation and radiomics survival prediction: Contribution to the brats 2017 challenge." International MICCAI Brainlesion
Workshop. Springer, Cham, 2017.
[5] Liu, Guilin, et al. "Image inpainting for irregular holes using partial convolutions." Proceedings of the European Conference on Computer Vision (ECCV). 2018.
07
Introduction/ Materials & Methods / Results / Discussions & Conclusion](https://image.slidesharecdn.com/strokersna1-201025173754/85/Deep-Learning-based-Fully-Automated-Detection-and-Quantification-of-Acute-Infarcts-8-320.jpg)
![Materials and Methods
Training Details
Large-size Lesion
Small-size Lesion
• Divide train dataset into two subsets w.r.t lesion size.
• Train two separate models for each subset of train
dataset and ensemble the results to get final
prediction.
• Use data augmentation, including rescaling,
rotation, horizontal flip, and x/y translation.
• Use Generalized Dice Loss with different class
weights to cope with imbalanced data (background
is much more dominant than the stroke lesion)
• Train for 100 epochs using cosine-annealing, with
minimum learning rate set to 2e-4. Adam optimizer
with weight decay of 1e-5 is used.
08
Generalized Dice Loss
* r - reference foreground segmentation
* p - predicted probabilistic map
[6] Sudre, Carole H., et al. "Generalised dice overlap as a deep learning loss function for highly unbalanced segmentations." Deep learning in medical image
analysis and multimodal learning for clinical decision support. Springer, Cham, 2017. 240-248.
[6]
Introduction/ Materials & Methods / Results / Discussions & Conclusion](https://image.slidesharecdn.com/strokersna1-201025173754/85/Deep-Learning-based-Fully-Automated-Detection-and-Quantification-of-Acute-Infarcts-9-320.jpg)