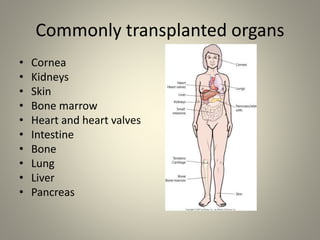
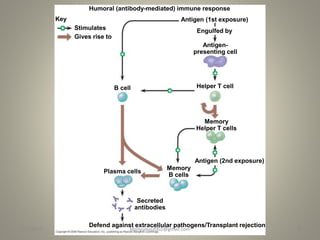
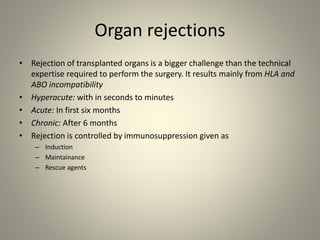
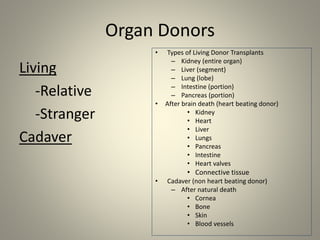
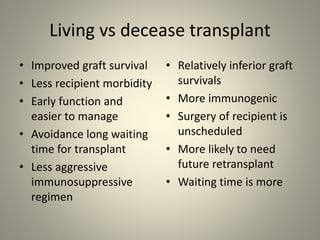
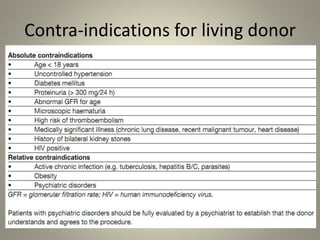
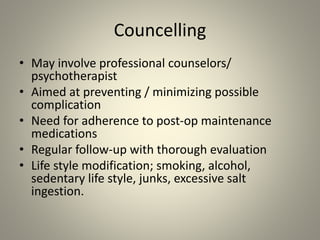
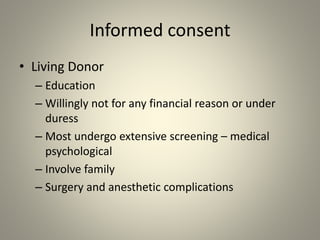
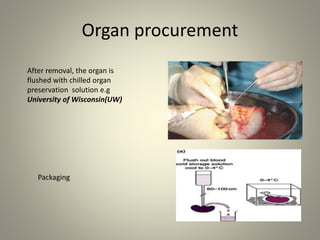
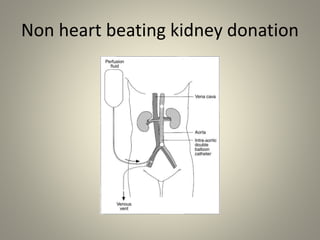
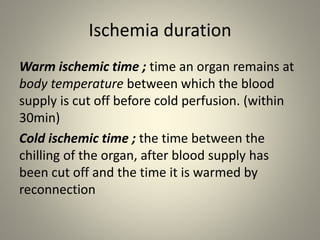
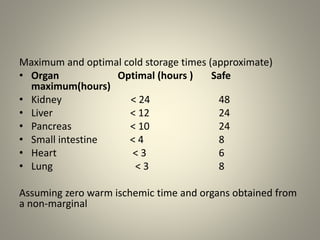
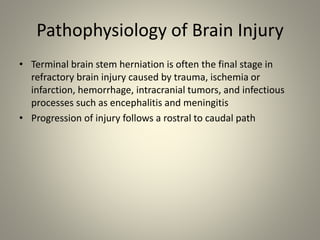
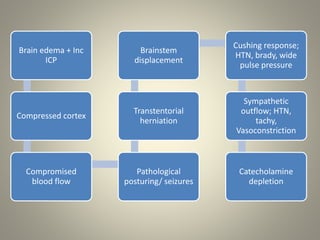
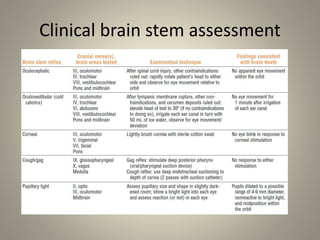
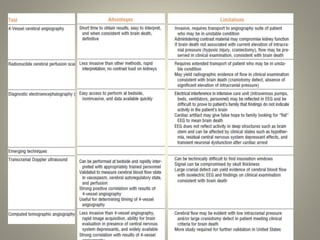
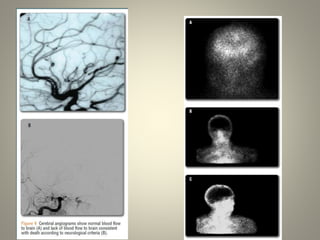
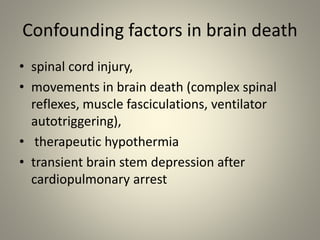
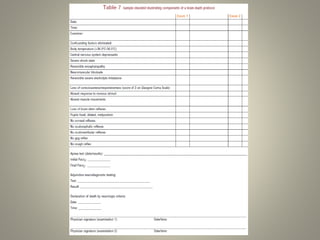
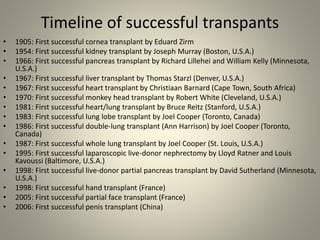
The document discusses deceased organ donation and transplantation. It covers organ sources like living and cadaver donors. Commonly transplanted organs are listed. Principles of transplantation include immune responses and types of rejection. Organ procurement involves removal and preservation. Brain death is required for deceased donation and involves loss of brain stem function. Ethical concerns around donation and a brief history of transplantation are also summarized.