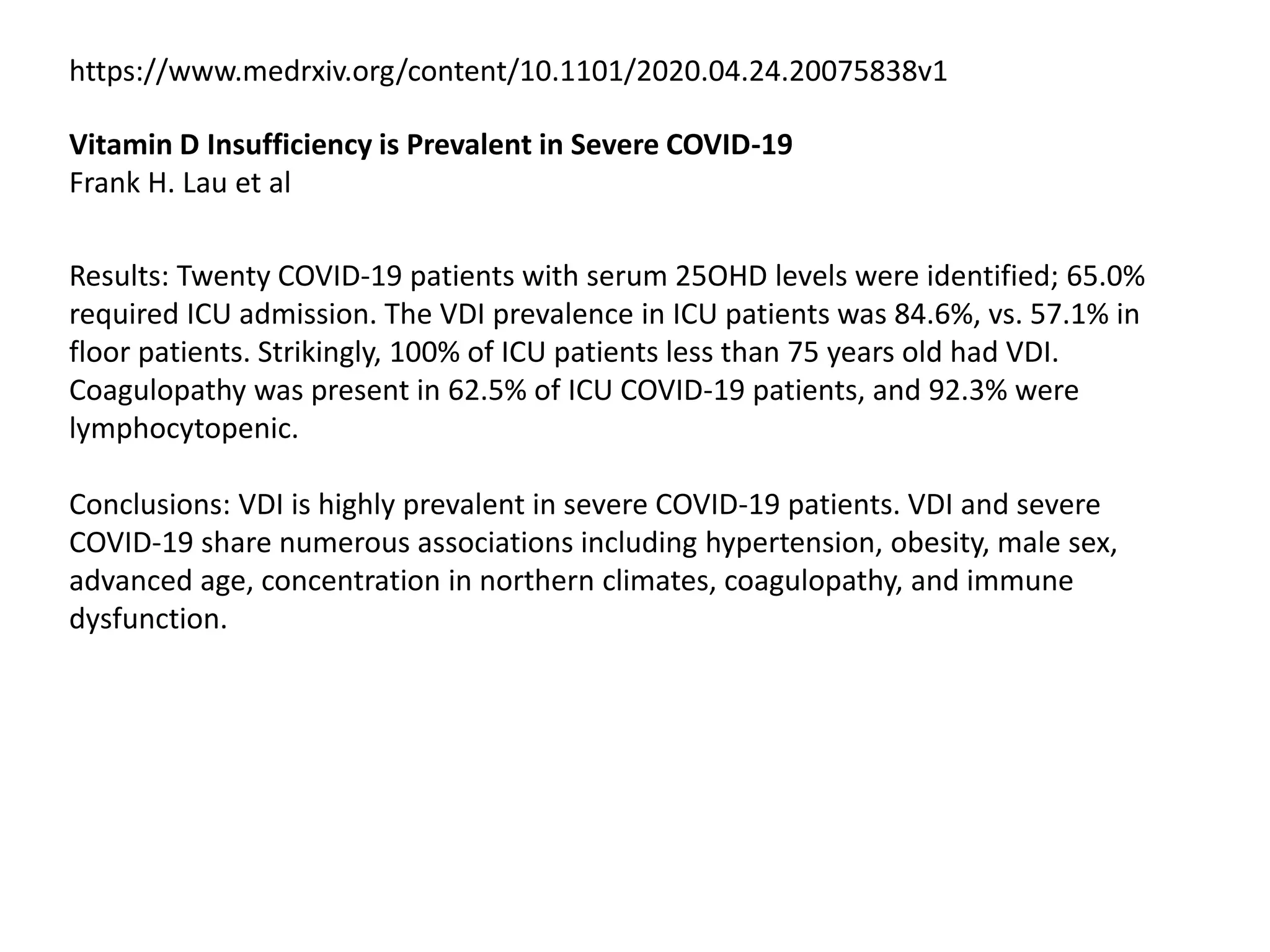
The document summarizes several studies that found associations between vitamin D deficiency and worse outcomes from COVID-19:
- Studies found higher rates of vitamin D deficiency in severe COVID-19 patients requiring ICU care compared to non-ICU patients. Deficiency was also linked to increased risk of COVID-19 infection and hospitalization.
- A study of over 4,000 COVID-19 patients found those with vitamin D deficiency at the time of testing had a higher risk of testing positive for COVID-19 compared to patients with sufficient levels.
- A study of older COVID-19 patients found those taking a combination of vitamin D, magnesium and B12 were less likely to require oxygen support or intensive care than those not



![https://www.medrxiv.org/content/10.1101/2020.05.08.20095893v1
Association of Vitamin D Deficiency and Treatment with COVID-19 Incidence
View ORCID ProfileDavid O Meltzer
Results: Among 4,314 patients tested for COVID-19, 499 had a vitamin D level in the
year before testing. Vitamin D status at the time of COVID-19 testing was categorized
as likely deficient for 127(25%) patients, likely sufficient for 291(58%) patients, and
uncertain for 81(16%) patients.
In multivariate analysis, testing positive for COVID-19 was associated with:
- increasing age(RR(age<50)=1.05,p<0.021;RR(age≥50)=1.02,p<0.064)),
- non-white race(RR=2.54,p<0.01) and
- being likely vitamin D deficient
- predicted COVID-19 rates in the vitamin D deficient group of 21.6%(95%CI[14.0%-
29.2%] ) versus 12.2%(95%CI[8.9%-15.4%]) in the vitamin D sufficient group.
- Conclusions and Relevance: Vitamin D deficiency that is not sufficiently treated is
associated with COVID-19 risk. Testing and treatment for vitamin D deficiency to
address COVID-19 warrant aggressive pursuit and study.](https://image.slidesharecdn.com/dcovidv3a-200707013711/75/D-covid-v3a-4-2048.jpg)
![https://www.medrxiv.org/content/10.1101/2020.07.01.20144329v1.full.pdf
Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an
Israeli population-based study
Eugene Merzon et al
14,000 members of Leumit Health Services who were tested for COVID-19 infection from February
1st to April 30th 2020, and who had at least one previous blood test for plasma 25(OH)D level.
"Suboptimal" or "low" plasma 25(OH)D level was defined as plasma 25-hydroxyvitamin D, or
25(OH)D, concentration below 30 ng/mL.
RESULTS:
Of 7,807 individuals, 782 (10.1%) were COVID-19-positive, and 7,025 (89.9%) COVID-19-negative.
The mean plasma vitamin D level was significantly lower among those who tested positive than
negative for COVID-19 [19.00 ng/mL (95% confidence interval [CI] 18.41-19.59) vs. 20.55 (95% CI
20.32-20.78)]. Univariate analysis demonstrated an association between low plasma 25(OH)D level
and increased likelihood of COVID-19 infection [crude odds ratio (OR) of 1.58 (95% CI 1.24-2.01,
p<0.001)], and of hospitalization due to the SARS-CoV-2 virus [crude OR of 2.09 (95% CI 1.01- 4.30,
p<0.05)].
In multivariate analyses that controlled for demographic variables, and psychiatric and somatic
disorders, the adjusted OR of COVID-19 infection [1.45 (95% CI 1.08-1.95, p<0.001)], and of
hospitalization due to the SARS-CoV-2 virus [1.95 (95% CI 0.98-4.845, p=0.061)] were preserved.
In the multivariate analyses, age over 50 years, male gender and low-medium socioeconomic status
were also positively associated with the risk of COVID-19 infection; age over 50 years was positively
associated with the likelihood of hospitalization due to COVID-19.
Conclusion: Low plasma 25(OH)D level appears to be an independent risk factor for
COVID-19 infection and hospitalization.](https://image.slidesharecdn.com/dcovidv3a-200707013711/75/D-covid-v3a-5-2048.jpg)