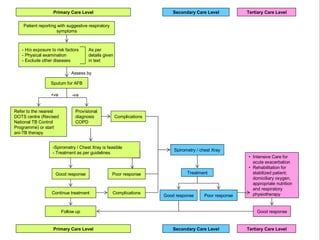
This document discusses chronic obstructive pulmonary disease (COPD), including its diagnosis, treatment according to severity, and management. The key points are:
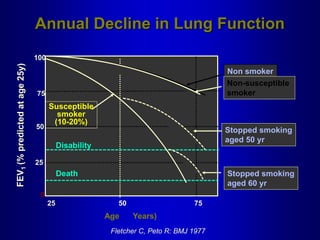
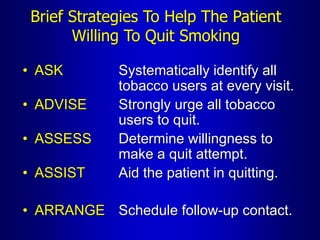
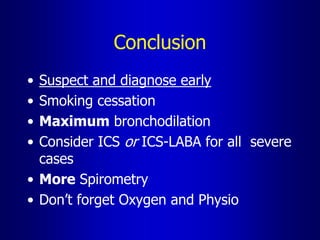
1. COPD is often missed or misdiagnosed. Early diagnosis, controlling symptoms, improving exercise tolerance, and reducing exacerbations are aims of treatment.
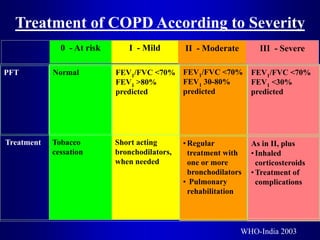
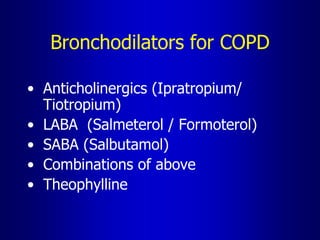
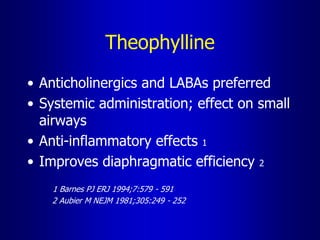
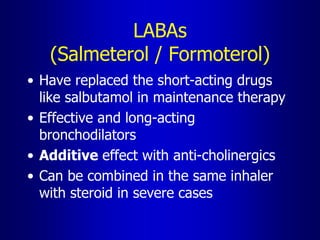
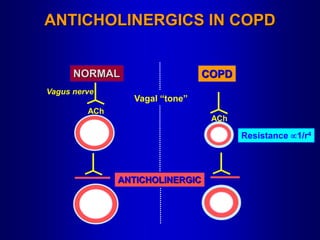
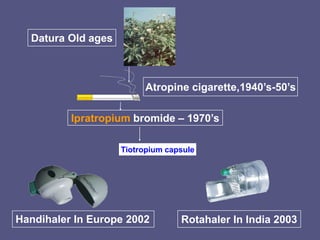
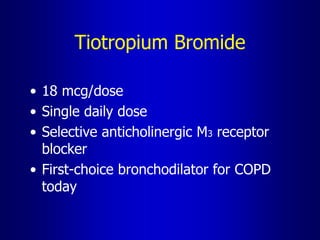
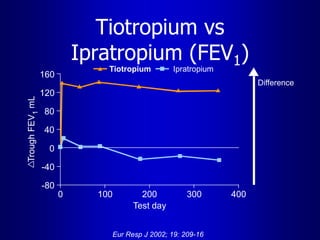
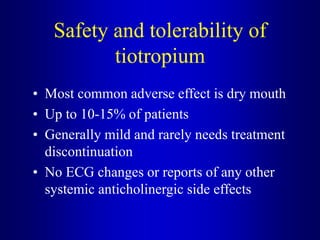
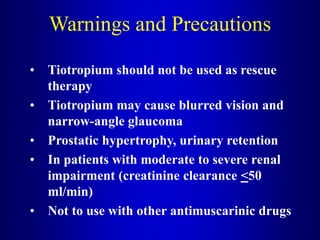
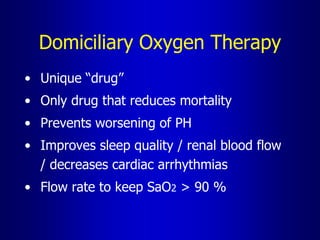
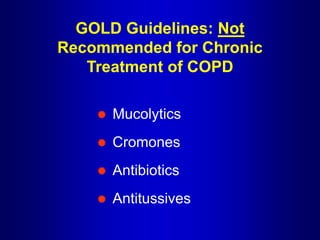
2. Treatment follows GOLD guidelines and depends on severity, ranging from risk reduction to long-term oxygen therapy. Bronchodilators are the cornerstone of drug therapy.
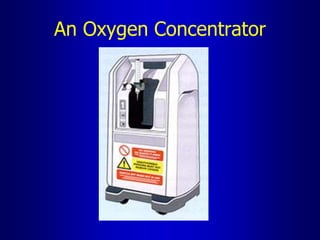
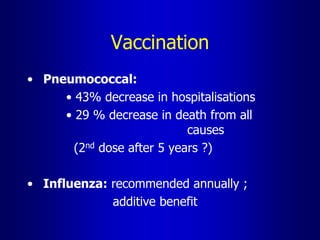
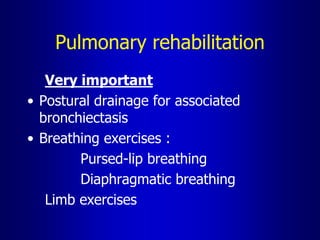
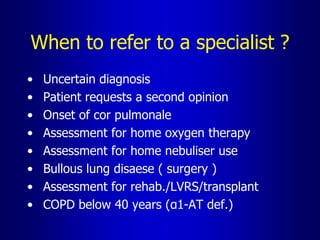
3. Other treatment considerations discussed include inhaled corticosteroids, pulmonary rehabilitation, oxygen therapy, vaccinations, and referral to specialists for complications or uncertain diagnosis. Proper diagnosis and management can improve patients' quality