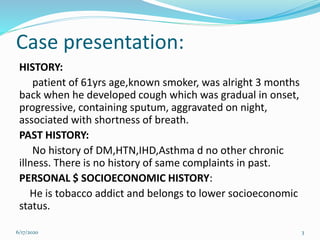
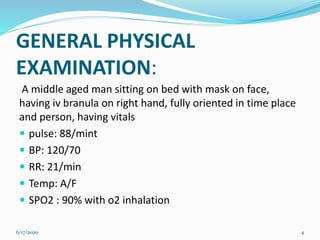
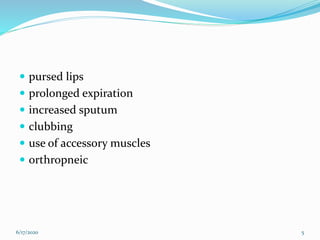
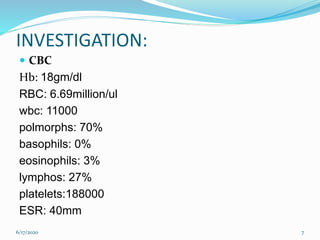
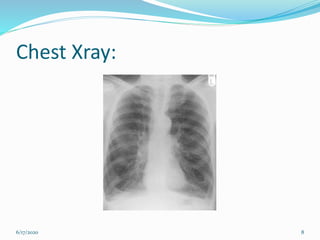
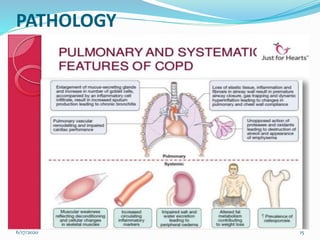
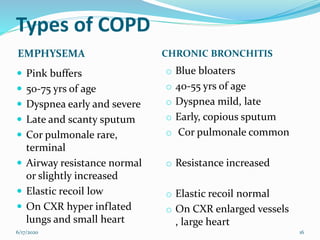
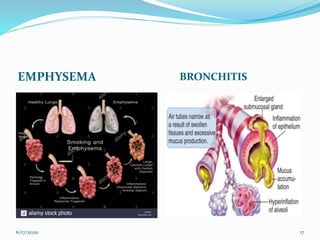
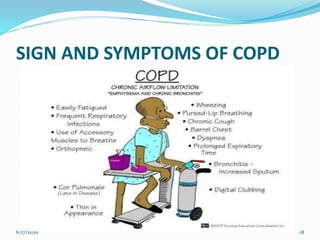
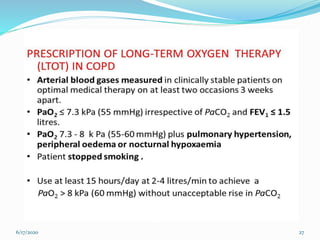
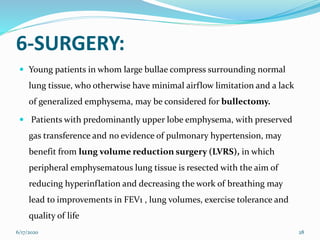
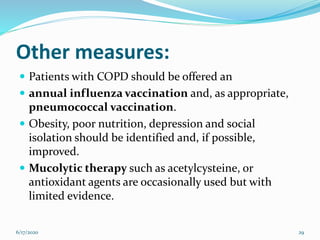
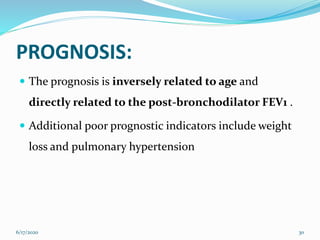
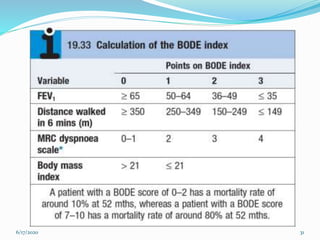
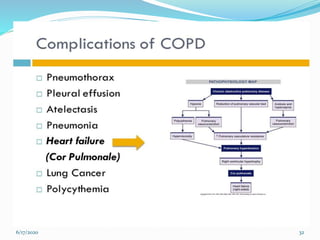
The document provides details on a case presentation of a 61-year-old male smoker with cough and shortness of breath. It then discusses the objectives, epidemiology, aetiology, risk factors, pathology, clinical features, investigations, management, and complications of chronic obstructive pulmonary disease (COPD). Key points include that COPD is caused by noxious particles like cigarette smoke damaging the lungs. Symptoms include cough, sputum production, and shortness of breath. Spirometry is used to diagnose and classify COPD severity. Management involves smoking cessation, bronchodilators, pulmonary rehabilitation, oxygen therapy, and occasionally surgery.