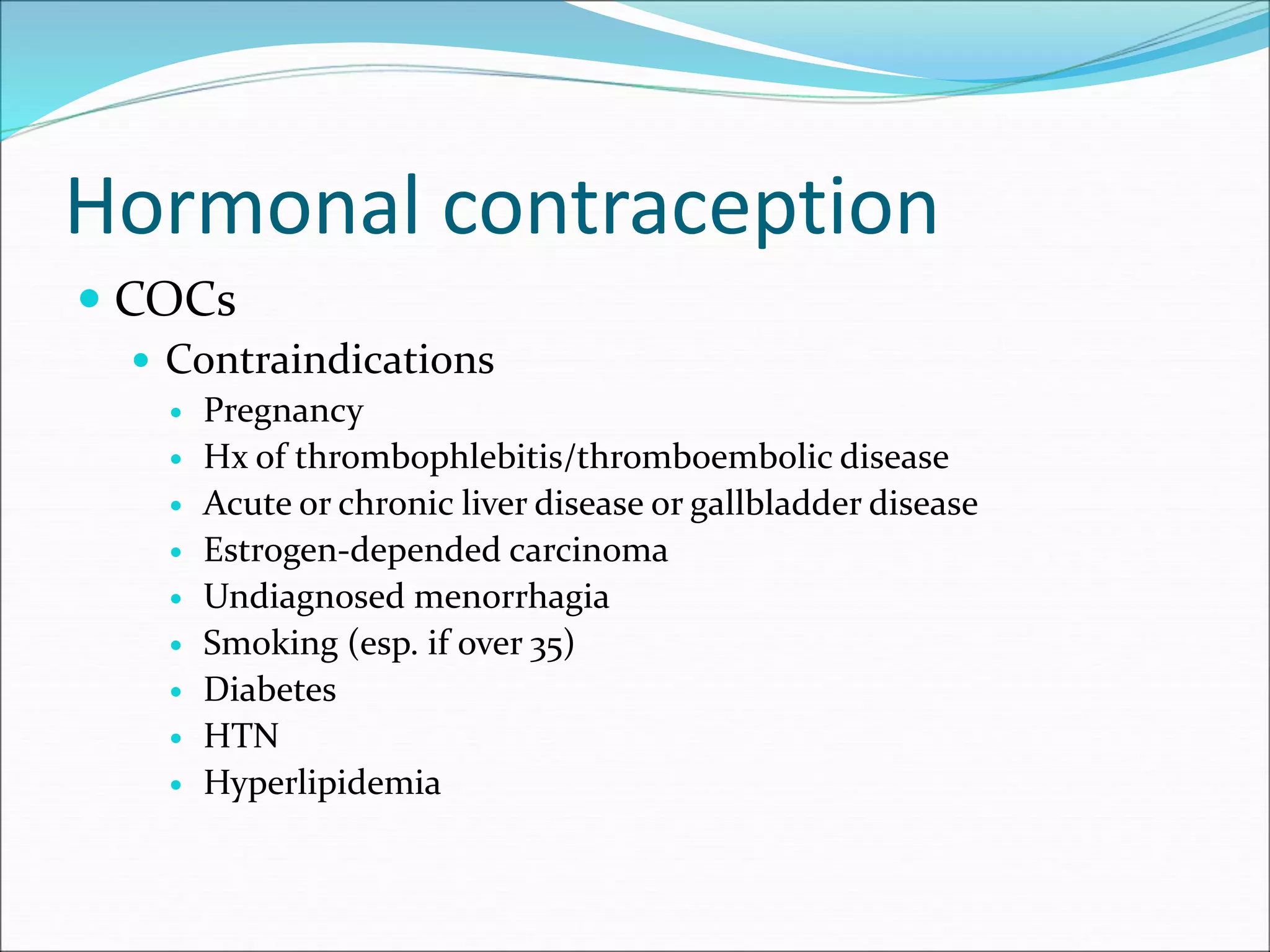
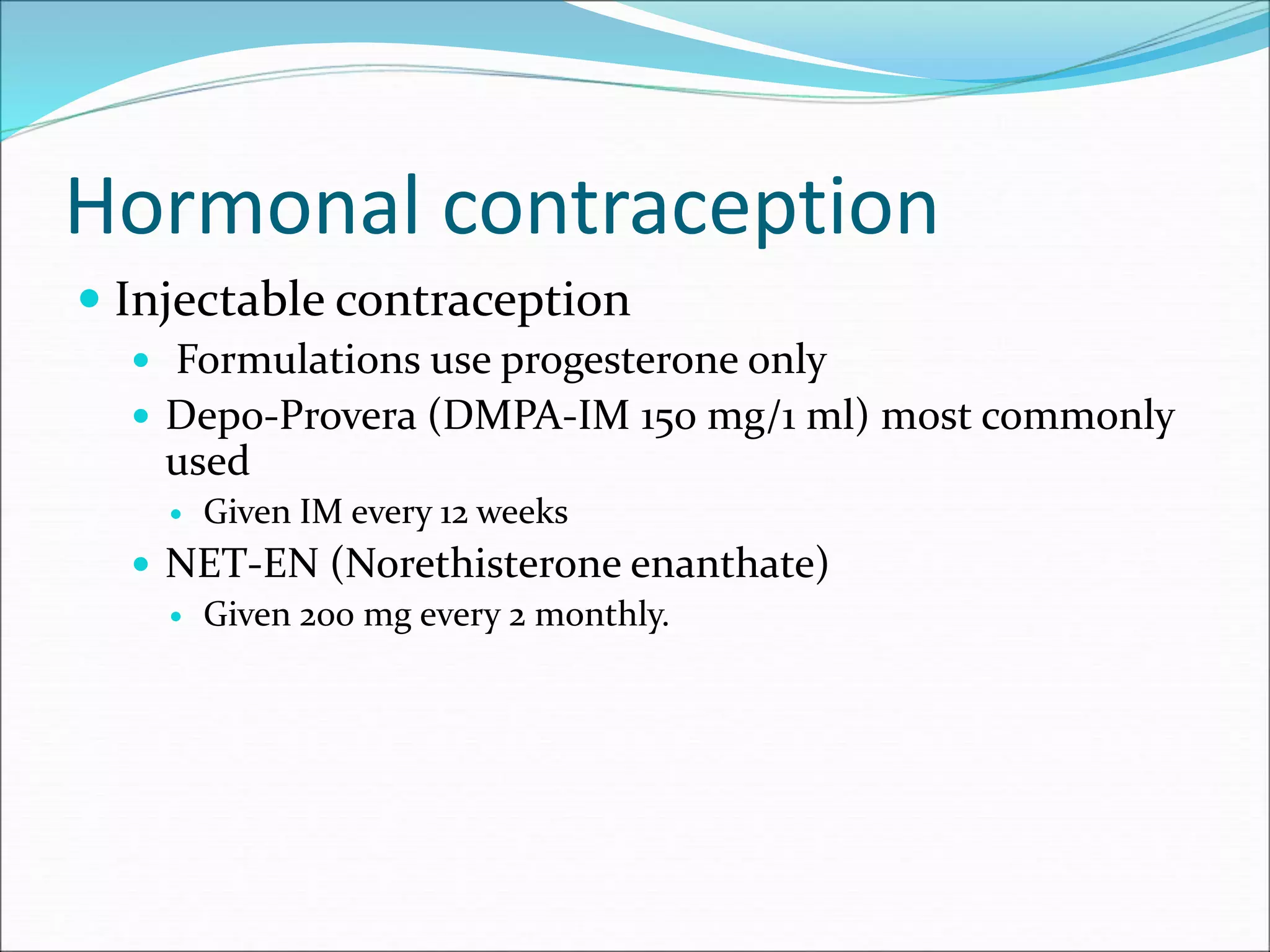
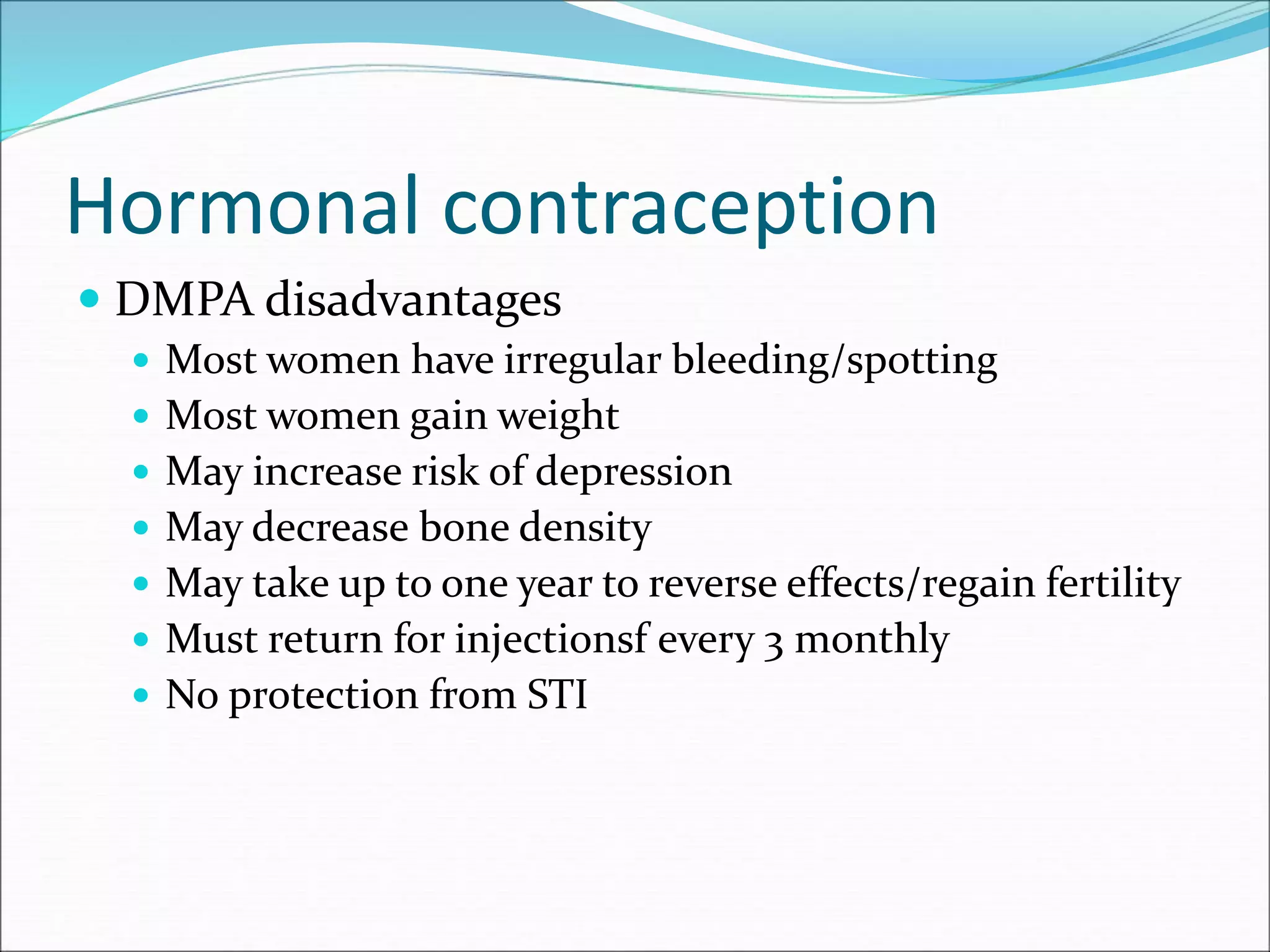
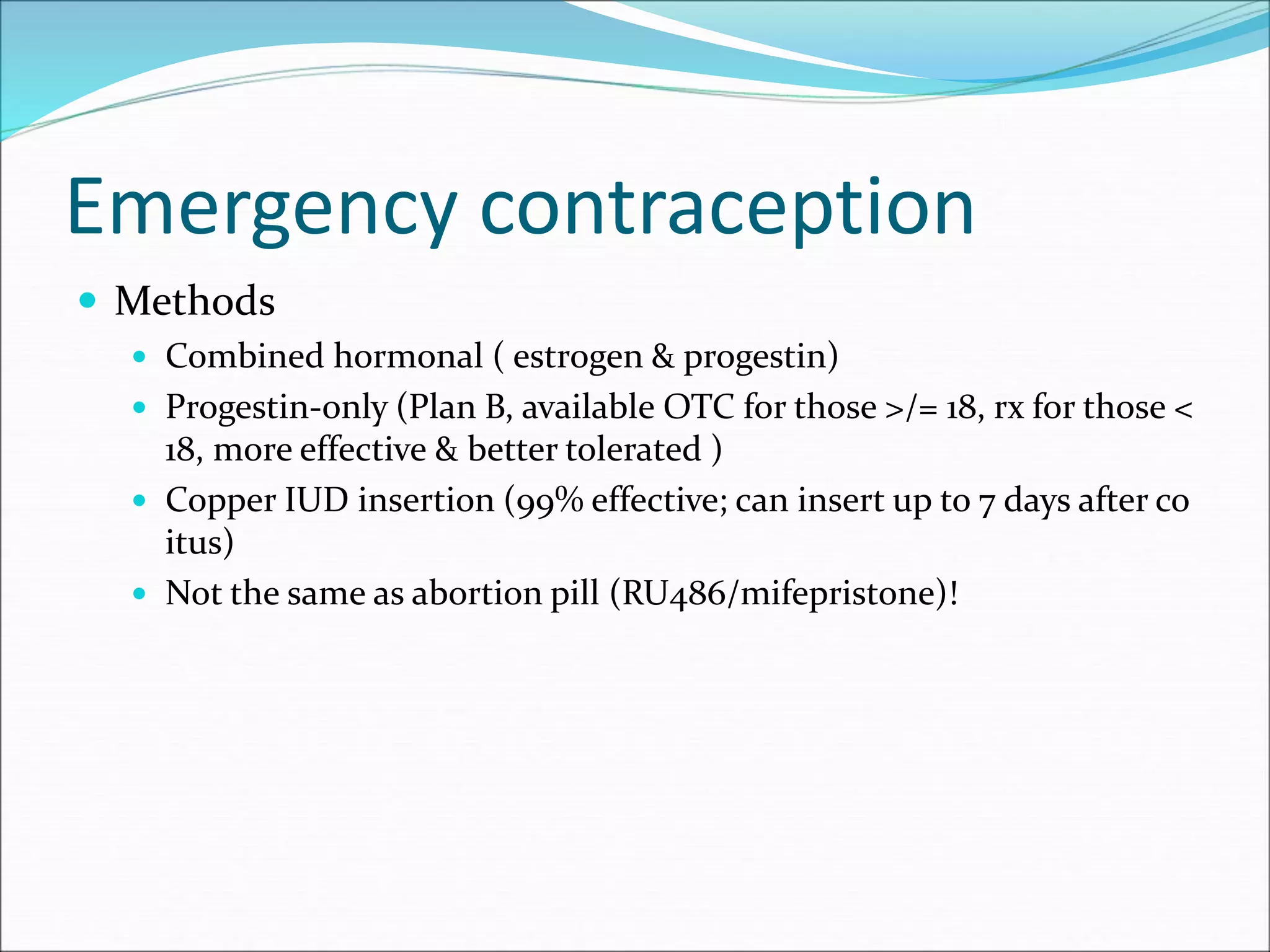
This document discusses various methods of contraception, including fertility awareness methods like basal body temperature tracking and cervical mucus monitoring, barrier methods like condoms and diaphragms, hormonal options like combined oral contraceptives and IUDs, and sterilization. It provides details on how each method works, effectiveness rates, potential side effects, and other important factors to consider when choosing a contraceptive approach.