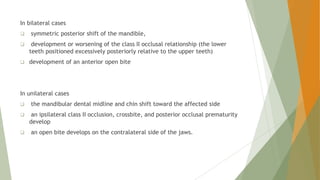
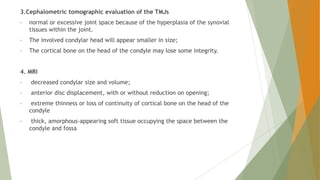
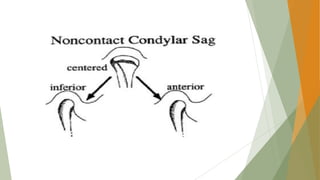
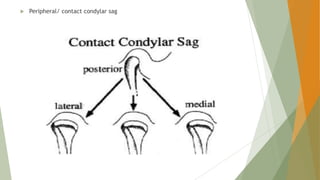
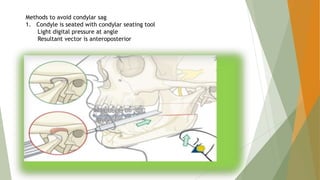
This document discusses condylar resorption and condylar sag, which are temporomandibular joint disorders. Condylar resorption involves the breakdown of the mandibular condyles through bone resorption and can be bilateral or unilateral. It causes symptoms like jaw pain and malocclusion. Causes may be idiopathic or related to trauma, orthodontics, or systemic diseases. Diagnosis involves x-rays and MRI. Treatment ranges from nonsurgical to orthognathic surgery. Condylar sag occurs after jaw surgery when the condyle shifts in the fossa, disrupting occlusion. Methods to avoid it include proper condyle seating and waking patients during surgery