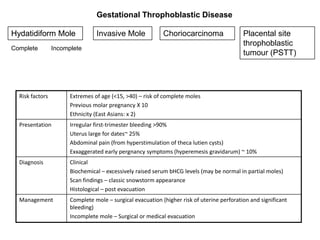
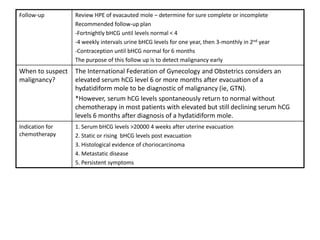
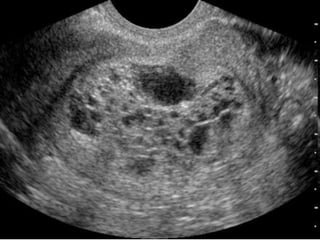
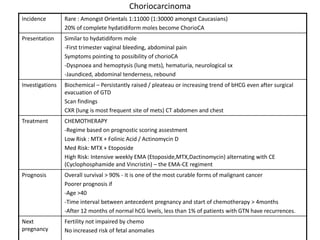
Gestational trophoblastic disease includes complete and partial hydatidiform moles, invasive moles, choriocarcinoma, and placental site trophoblastic tumors, with molar pregnancies requiring surgical evacuation and strict follow up of beta HCG levels to monitor for malignant transformation into gestational trophoblastic neoplasia. Risk factors include extremes of maternal age, previous molar pregnancies, and ethnicity, while presentation is typically irregular bleeding and an enlarged uterus out of proportion to gestational age.