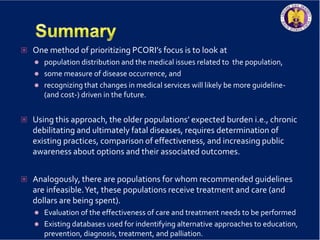
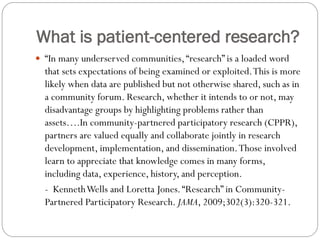
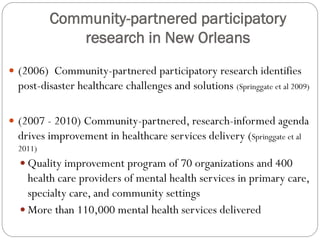
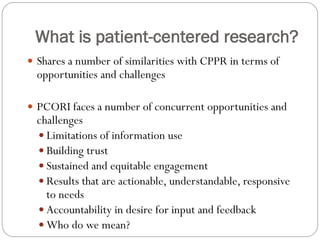
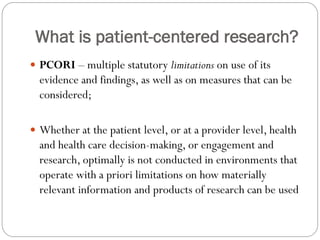
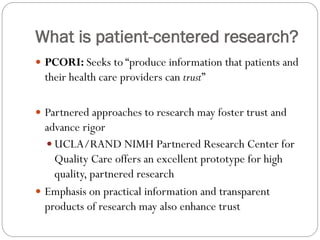
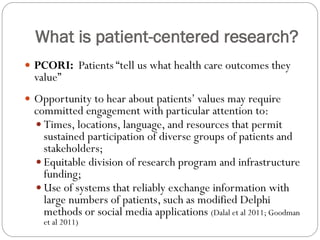
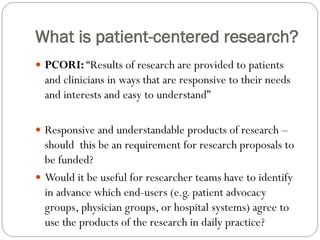
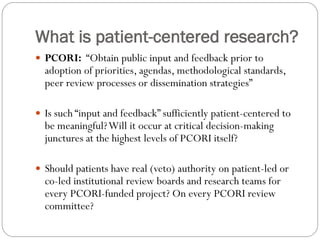
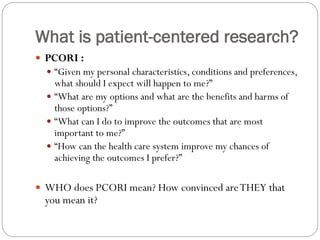
The document discusses patient-centered research, particularly focusing on community-partnered participatory research (CPPR) and its role in addressing healthcare challenges in underserved populations. It highlights the importance of collaborative approaches that involve patients and stakeholders in decision-making, and outlines the challenges faced by organizations like PCORI in producing trustworthy and actionable health information. Additionally, it emphasizes the need for equitable engagement and responsive communication in health research to enhance patient outcomes and trust.

![Patient Concerns:
Patients may not know what to ask providers, or may feel
uncomfortable about “challenging” providers. [Patients
must overcome their personal barriers to managing their
disease successfully, which they may perceive as severe
and numerous.]
http://www.qualityprofiles.org/leadership_series/diabete
s/diabetes_addressing_quality_gaps.asp
Older patients’ health problems do not occur only during
“office hours” (i.e., Monday-Friday, 9am-5pm). Older
patients are usually told to go to an emergency room on
Friday, Saturday, or Sunday, which is less than ideal.](https://image.slidesharecdn.com/combinedpowerpoints-130805101346-phpapp01/85/Board-of-Governors-Meeting-New-Orleans-27-320.jpg)