This document provides a toolkit for new leaders in developing collaborative healthcare teams. It contains 5 modules that address key topics for building effective interprofessional teams. The first module discusses leadership concepts and styles that are important for leading teams, such as transformational leadership that focuses on relationships and empowering individuals. It also identifies qualities of effective leaders, including being able to learn and adapt to different situations. The module provides guidance for new healthcare leaders on developing strong leadership to establish collaborative teams.













![i. Past Experiences with Power20
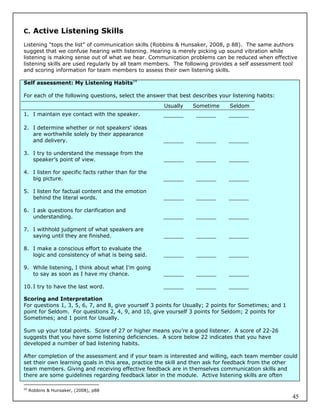
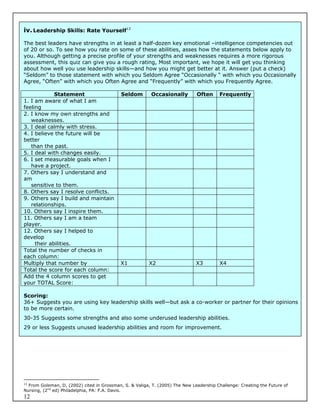
Objectives:
1. To revisit experiences with power
2. To distinguish elements that contribute to positive or negative feelings about power
3. To create an initial foundation for further discussions of the concept of power
Materials needed:
Chart paper
Felt pens
Individually write down one example of a time when you observed or experienced power being used in
a positive or productive manner. You may have observed this in person, on television, from afar, or
actually used your power in this way. After you note this experience, write down what it was about this
experience that caused you to remember it as productive and positive?
Then, write down one example of a time when you observed or experienced power being used in a
negative, disrespectful or destructive way. Again, this may have been power observed or experienced
in person, on television or from afar. Note what caused you to remember this experience as negative.
In your [small] group, share the details and reactions to both of these experiences. On one piece of
chart paper, collate the elements that comprised positive experiences. On another piece of chart paper,
collate the elements that comprised negative experiences. Each group will share its thoughts and
listings with the whole group and post. As a whole group, discuss whether the positive or negative
experiences have influenced your current views of power and why that might be.
20
McKinley, L. and Ross, H. (2008) You and Others Reflective Practice for Group Effectiveness in Human Services. Toronto:
Pearson Education.
18](https://image.slidesharecdn.com/collaborativeteamstoolkitmar2009drshabon-120820202121-phpapp01/85/Collaborative-teams-toolkit-mar-2009-dr-shabon-19-320.jpg)
![G. Leading Change
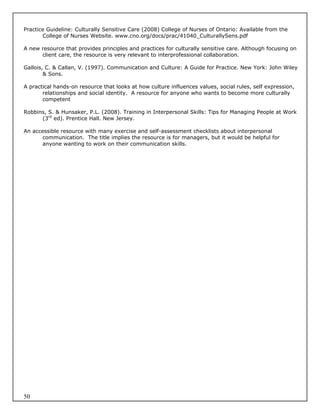
Leading change is frequently a challenge for leaders. If you are the leader of a new initiative, health
centre or family health team you are likely leading a change of some kind. The need to respond to
community needs and a rapidly changing policy environment as well as the tremendous challenges to
the health-care system means that change may be occurring at many levels within an organization,
often simultaneously. To help you think about the kind of change you are leading and the supports that
could be used by team members, you can consider whether the change is developmental, transitional
or transformational.21
Developmental change aims to change an existing situation or process through enhancement. This
type of change may seek to improve communication, team work or implement an improvement such as
a new process or technique. In developmental change the goal or desired outcome of the change is
clear. The leader supports developmental change by providing information that shares the rationale for
the needed change and by assisting with the setting of new goals that stretch team members while also
ensuring that the resources and support for meeting the new goal are in place.
Transitional change is characterized by the need to “replace what is with something entirely
different.”22 This order of change requires leaders to recognize that something completely different is
required in order to respond to an opportunity or challenge. Examples of transitional change include the
introduction of new programs or implementing new technologies that are similar to existing ones.
Transitional change may not require high levels of change from the people involved or within the
workplace culture. The leader uses clear communication, participation of the affected people and their
control over the implementation to achieve the desired new state. The leader supports transitional
change by identifying the differences between the existing and desired outcomes. The leader can
facilitate the identification of anything that can be brought forward to serve the new situation, what will
have to be left behind or is no longer needed, and what new components will be created to complete
the new state. This type of change is often implemented with a parallel structure: one to keep existing
operations going and another to manage the stages of planning and implementing the required
changes.
The third type of change is transformational change. This type of change is marked by high levels of
uncertainty and complexity that will require attitude, behaviour and cultural changes from all involved.
The final result or outcome may not be known and the “scope of this change [is] so significant that it
requires the organization’s culture and people’s behaviour and mindsets to shift fundamentally in order
to implement the changes successfully and succeed in the new state.”23 In transformational change,
the result emerges from a chaotic or unstable state. The leader’s role in transformational change is to
monitor all sources of feedback to continually assess the process and direction of the change and adjust
the course to continue in the desired direction. The leader becomes an adept learner to interpret and
act on the feedback and facilitates learning in others.
21
Anderson, D and Ackerman Anderson, L. (2001) Beyond Change Management: Advanced Strategies for Today’s
Transformational Leaders. Jossey/Bass – Pfeiffer.
22
Anderson and Ackerman Anderson, p. 35.
23
Anderson and Ackerman Anderson, p. 39.
19](https://image.slidesharecdn.com/collaborativeteamstoolkitmar2009drshabon-120820202121-phpapp01/85/Collaborative-teams-toolkit-mar-2009-dr-shabon-20-320.jpg)












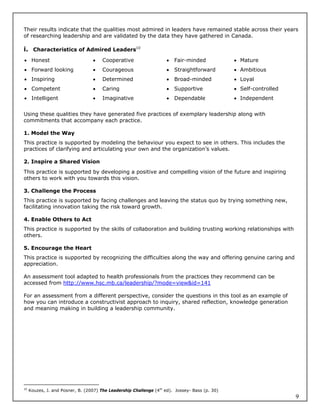
![1 2 3 4 5
We don’t have We have some objectives We have
either and/or some measures both
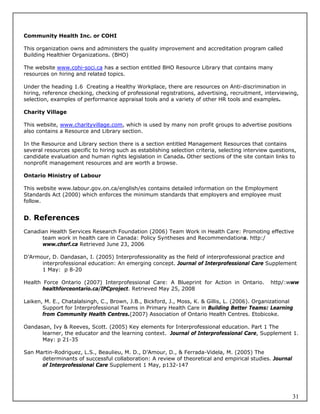
8. Empowerment plan: Does the team have a clear picture of which decisions it can make and which
require management approval?
1 2 3 4 5
There is no We are clear about We are clear about how
empowerment some items empowered we are
plan
9. Roles and responsibilities: Are you clear about what’s expected of you and how your role relates to
the roles of other team members?
1 2 3 4 5
I’m unclear I’m somewhat clear I’m totally clear
10. Communication plan: Does the team have a plan that describes who it should communicate with,
when, and how?
1 2 3 4 5
No plans Somewhat planned We have a plan
Comments:
Return the completed survey to:
[Insert contact information]
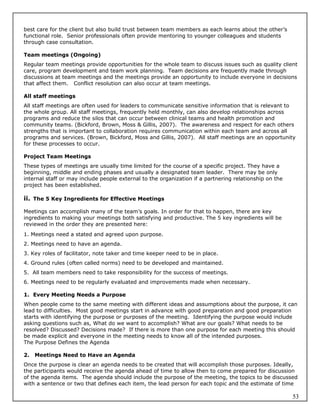
Team members seek opportunities to define roles and responsibilities during the team formation stage.
Team members “may be unclear about their expectations of each other, and group leader’s
expectations of them; and are probably unsure about the roles each of them will play in the work of the
group.”35 Team members will want to discuss their roles and responsibilities, often with a heavy
emphasis on their tasks. Some people respond to the uncertainty of the forming stage by “want[ing]
every task defined and allocated to someone and their own job, responsibilities and powers clearly
defined.”36 Payne cautions that this is a polarity: there may not be a right answer, rather, the team
needs to find a balance between too much uncertainty or too much constraint leading to unnecessary
bureaucracy. He suggests five categories for considering team priorities, specialization and workload
allocation and notes that in practice these categories are often combined with factors such as
geographic location and team member skills and interests to create a complex system for defining roles
and responsibilities:
legal requirements
types of work (for example, group work, cognitive-behavioural therapy)
service user categories (for example, client problems)
levels of risk, difficulty or complexity
organizational or political policies (for example, performance indicators)
C. Dimensions of Team Roles
35
Laiken, M. 1994)
36
Payne, M. (2000) p. 86.
34](https://image.slidesharecdn.com/collaborativeteamstoolkitmar2009drshabon-120820202121-phpapp01/85/Collaborative-teams-toolkit-mar-2009-dr-shabon-35-320.jpg)