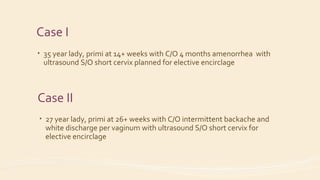
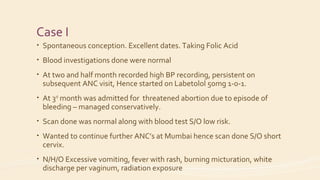
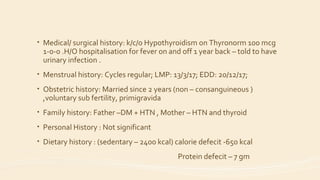
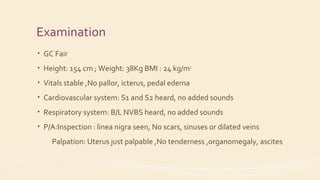
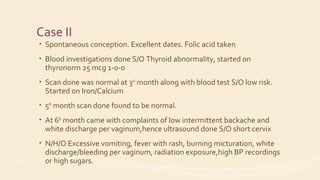
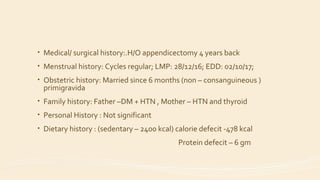
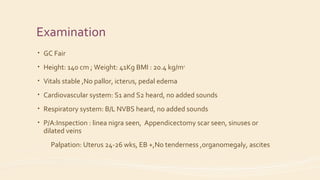
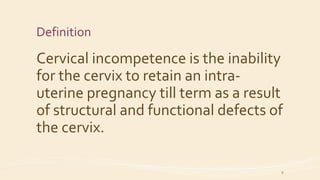
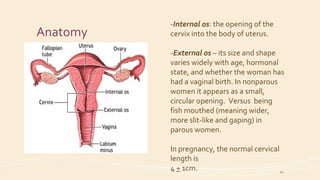
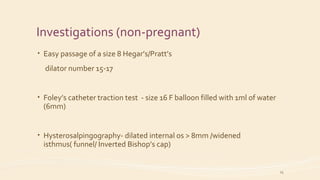
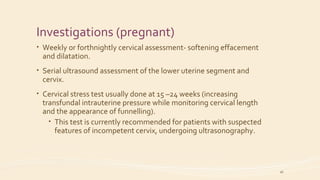
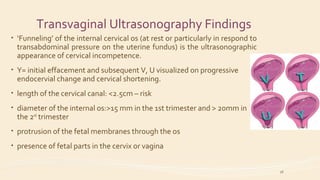
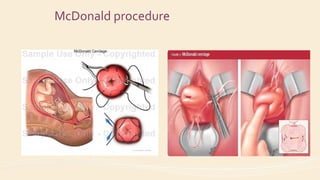
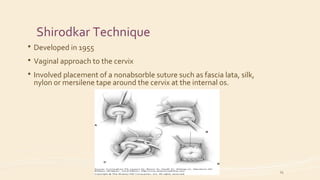
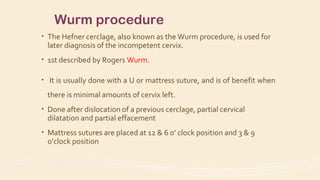
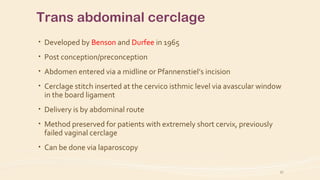
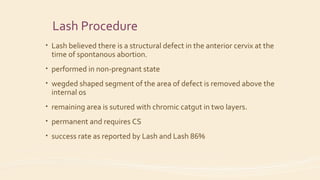
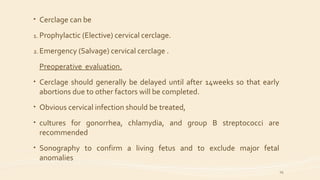
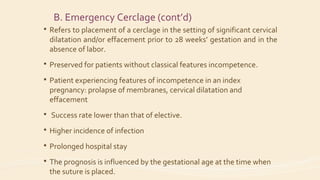
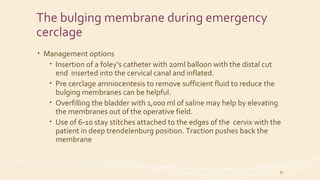
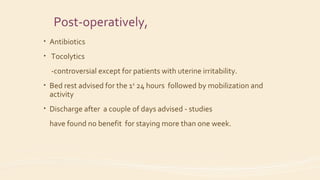
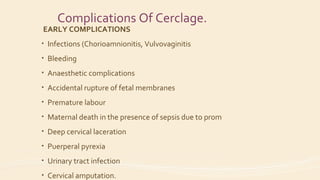
The document discusses cervical incompetence, detailing two case studies of pregnant women experiencing issues related to short cervical length and the management options, including elective cerclage. It covers definitions, pathogenesis, diagnosis, investigations, and surgical and medical interventions for cervical incompetence, highlighting the importance of timely intervention to improve outcomes. Additionally, various techniques for cervical cerclage and potential complications are explained.