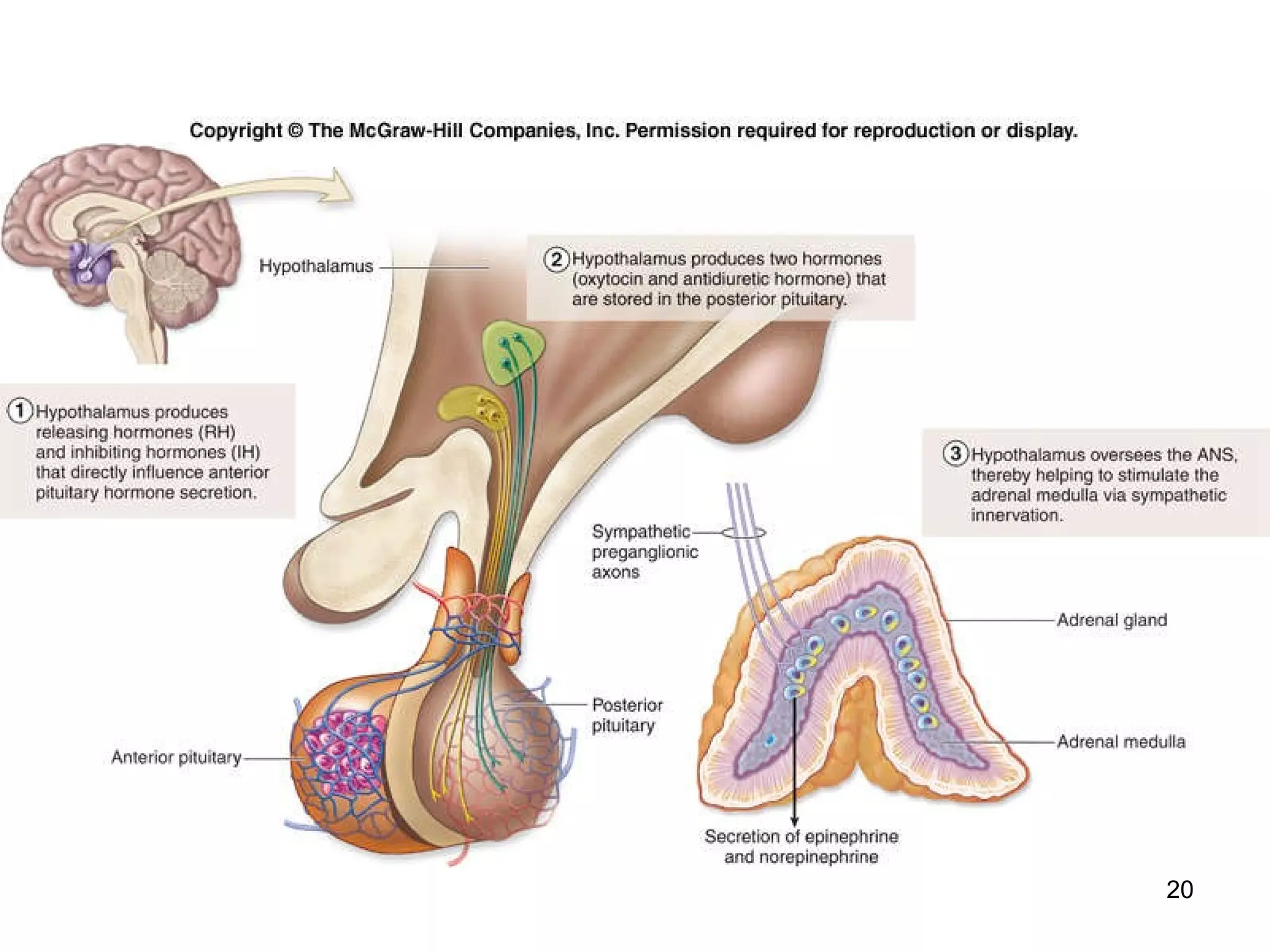
The document provides an overview of the endocrine system, including:
1) It discusses the differences between the nervous and endocrine systems in their communication methods, target organs, and effects.
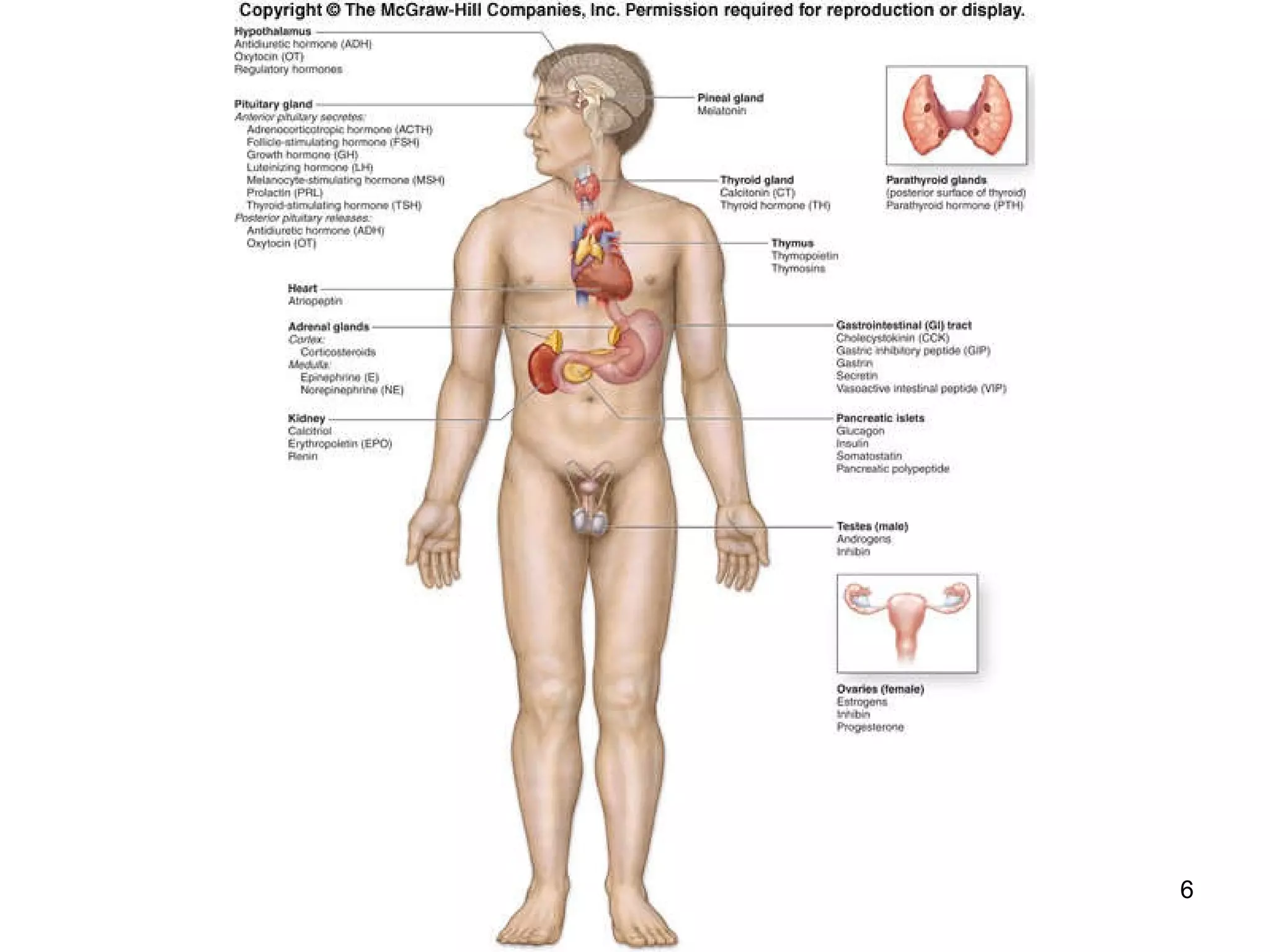
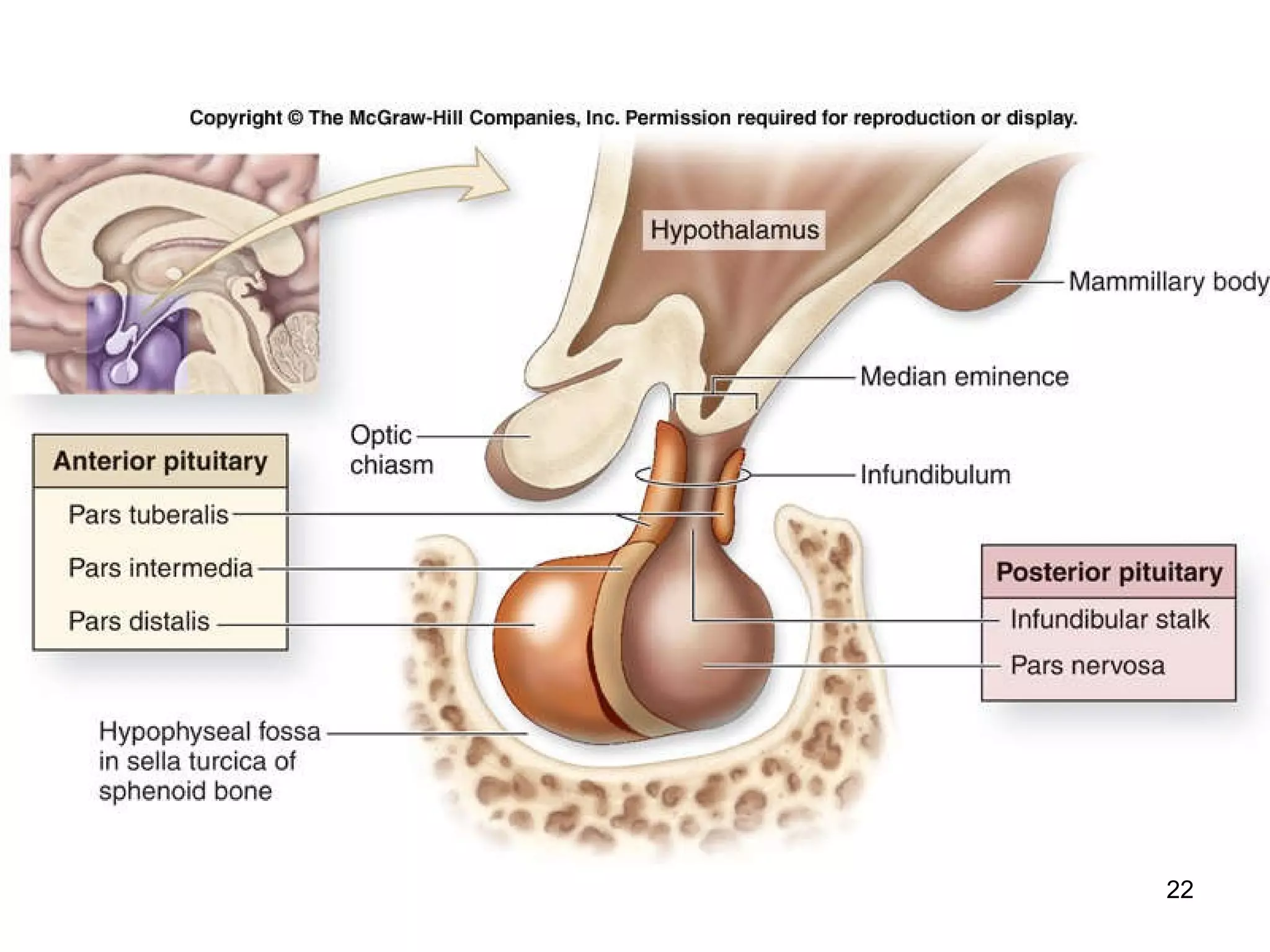
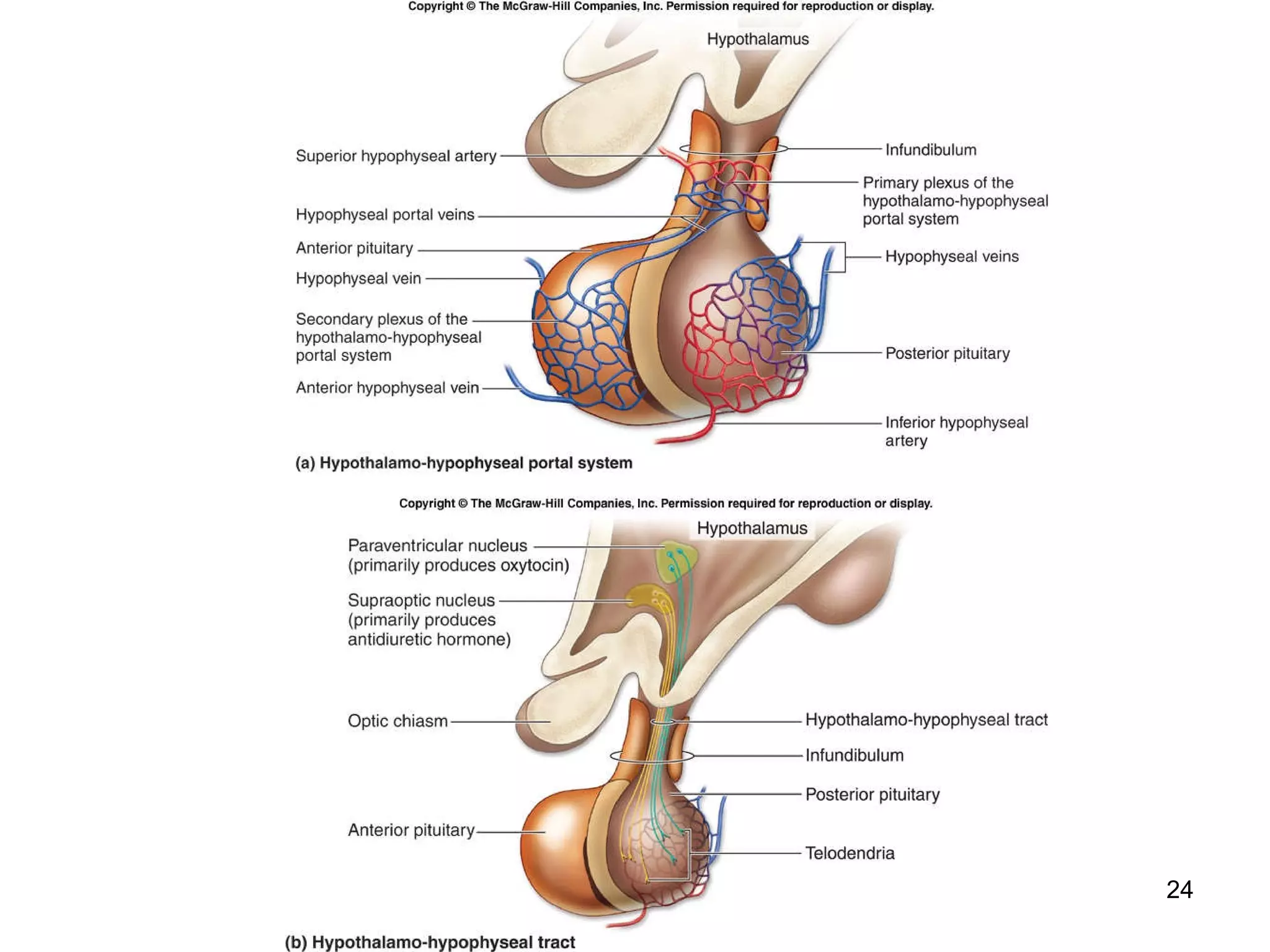
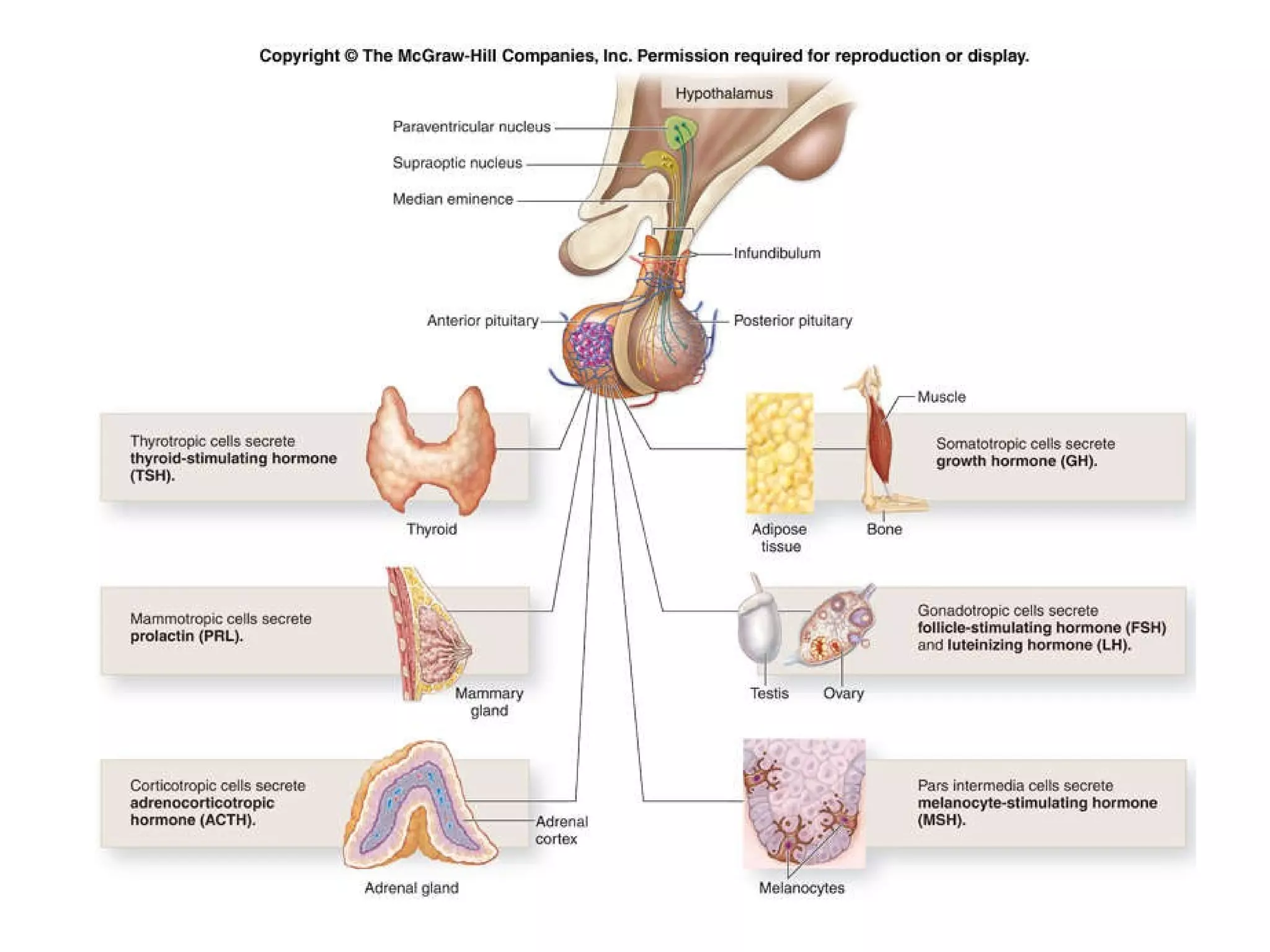
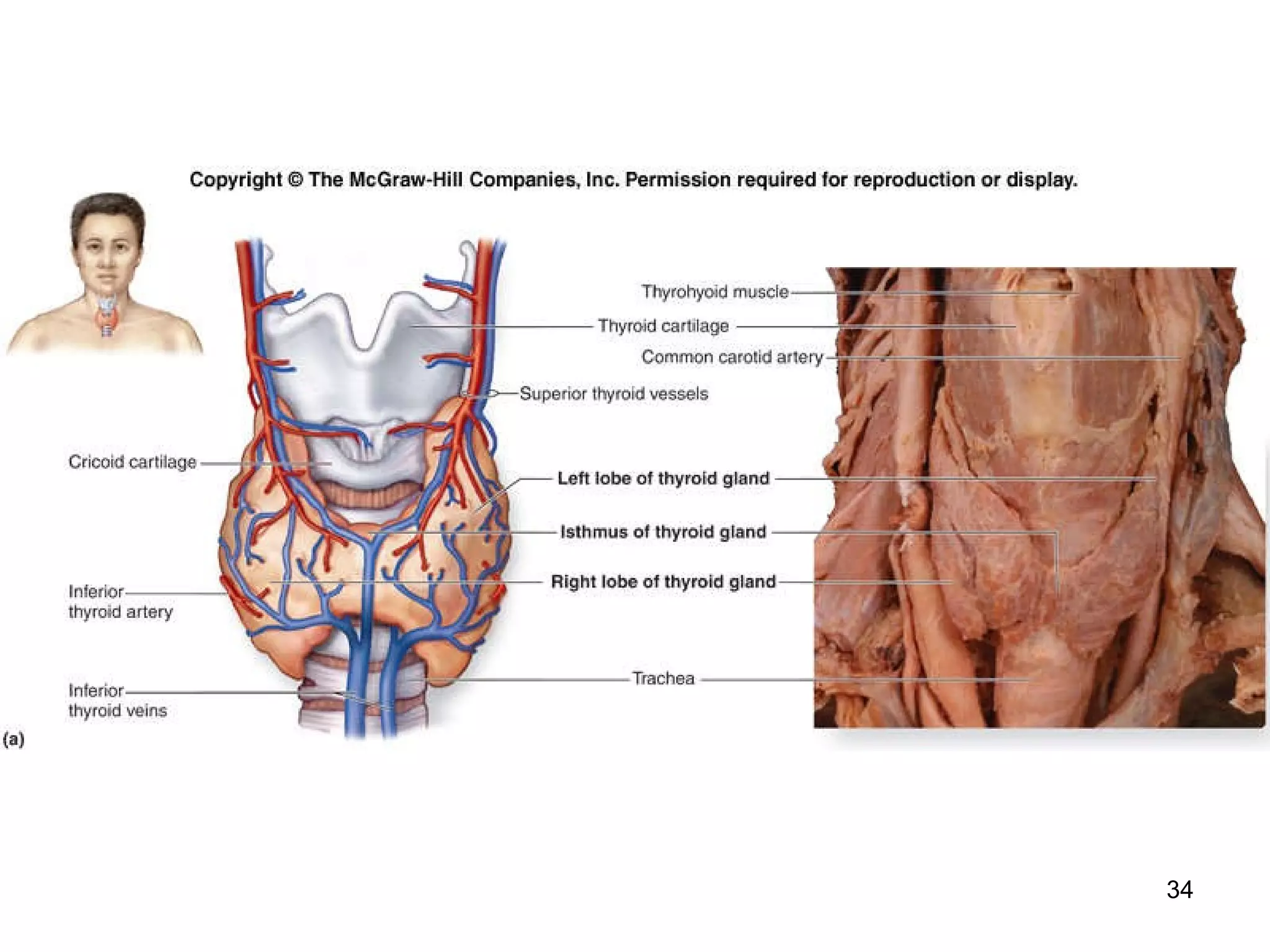
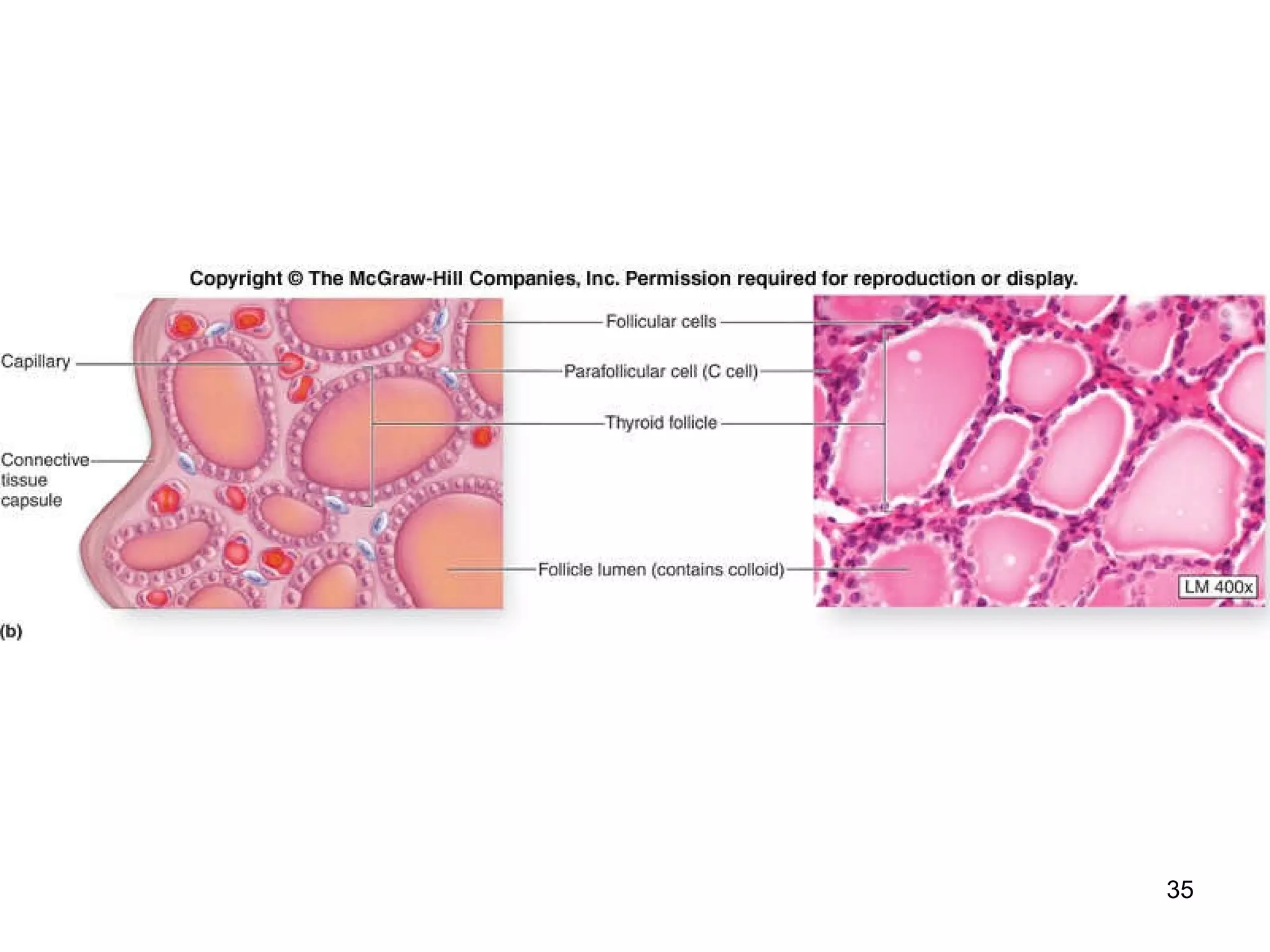
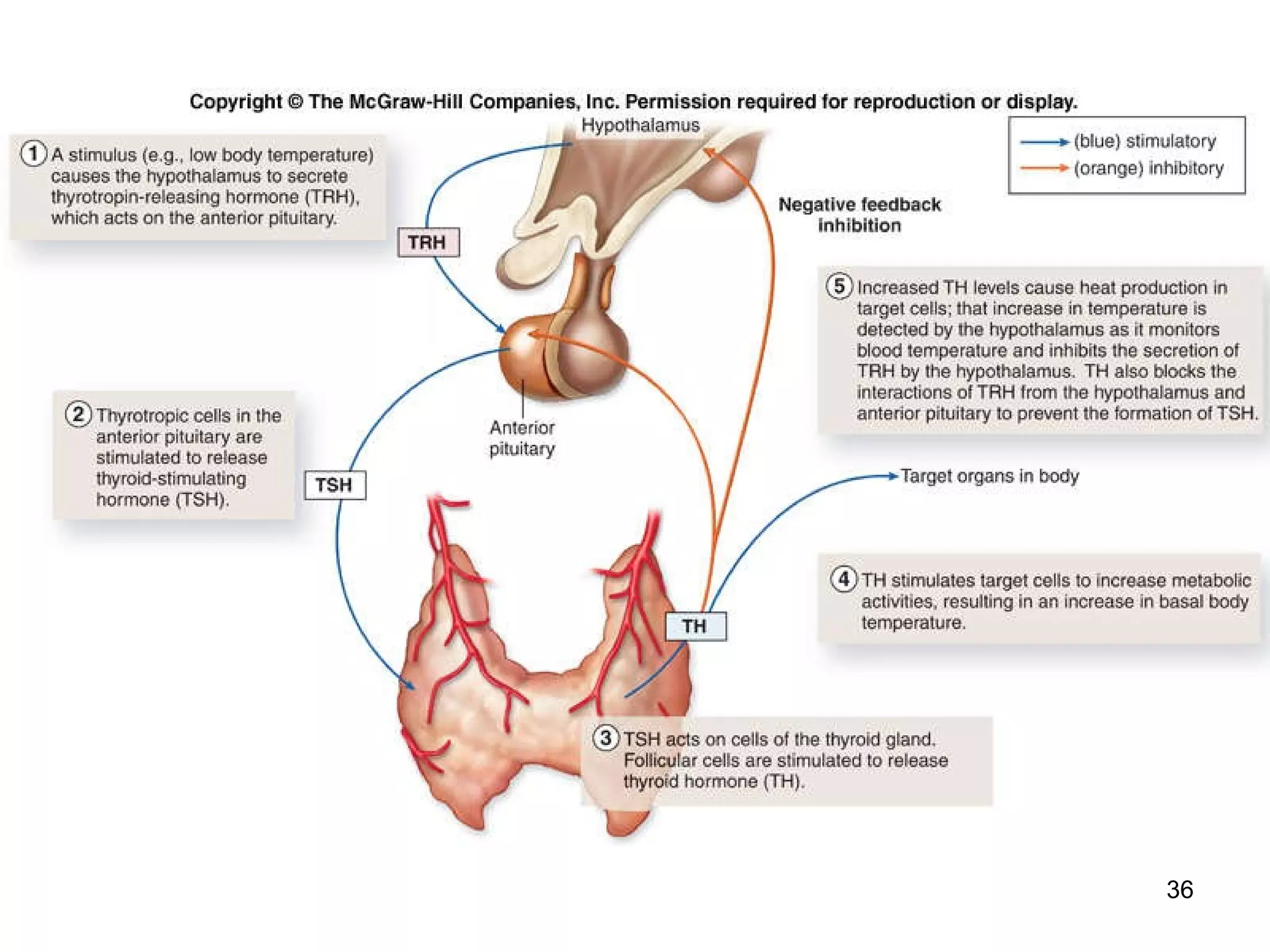
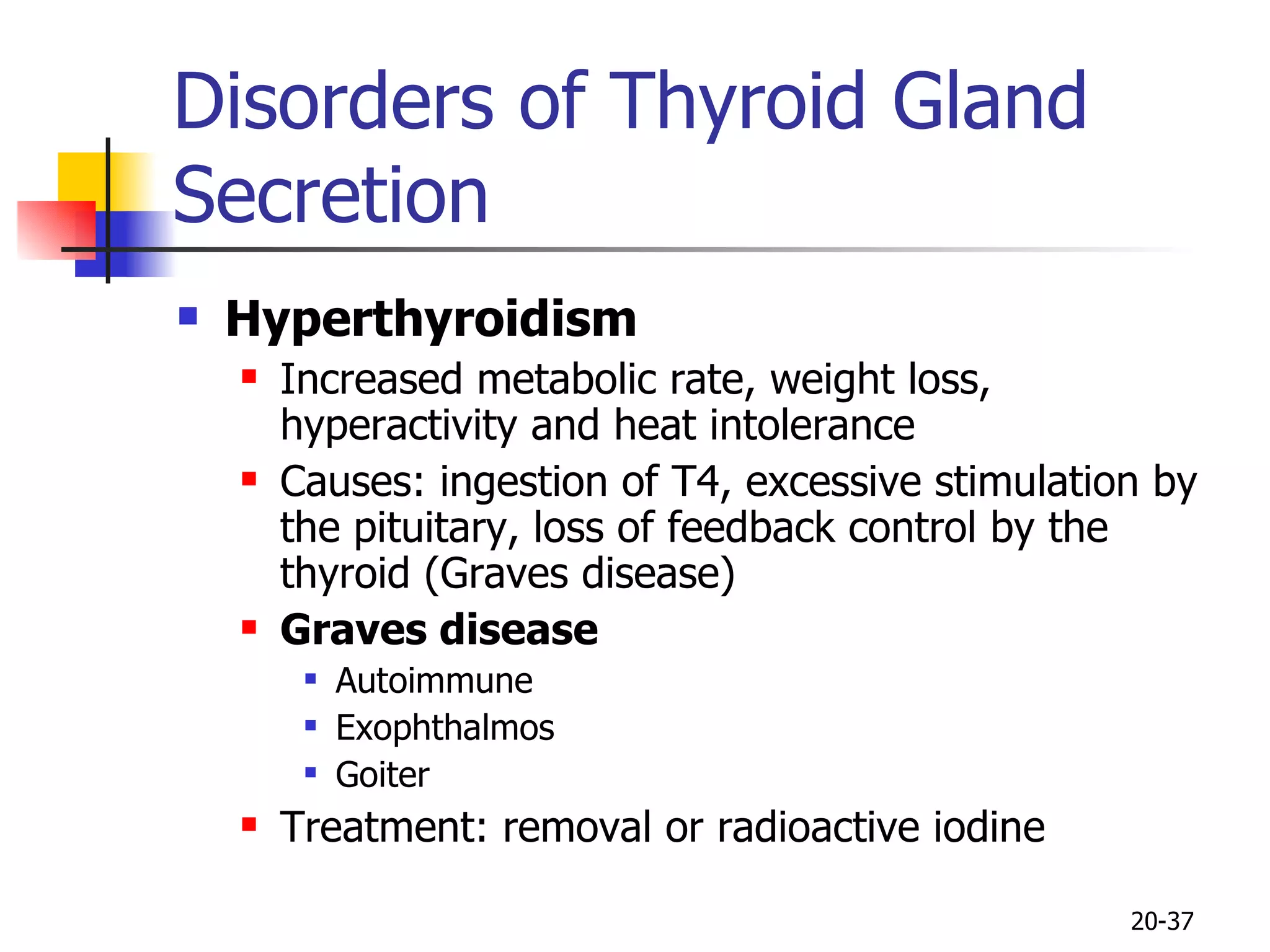
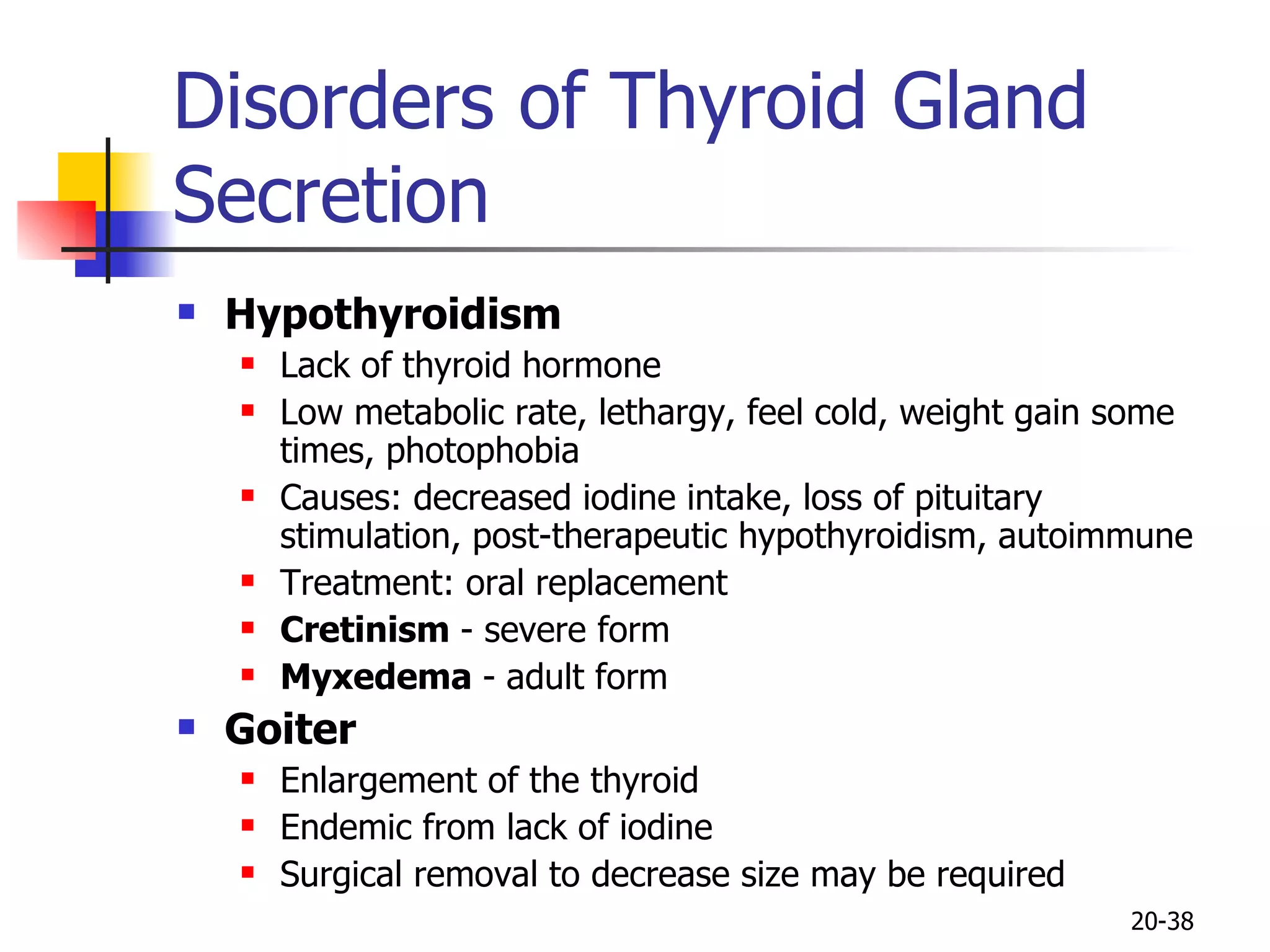
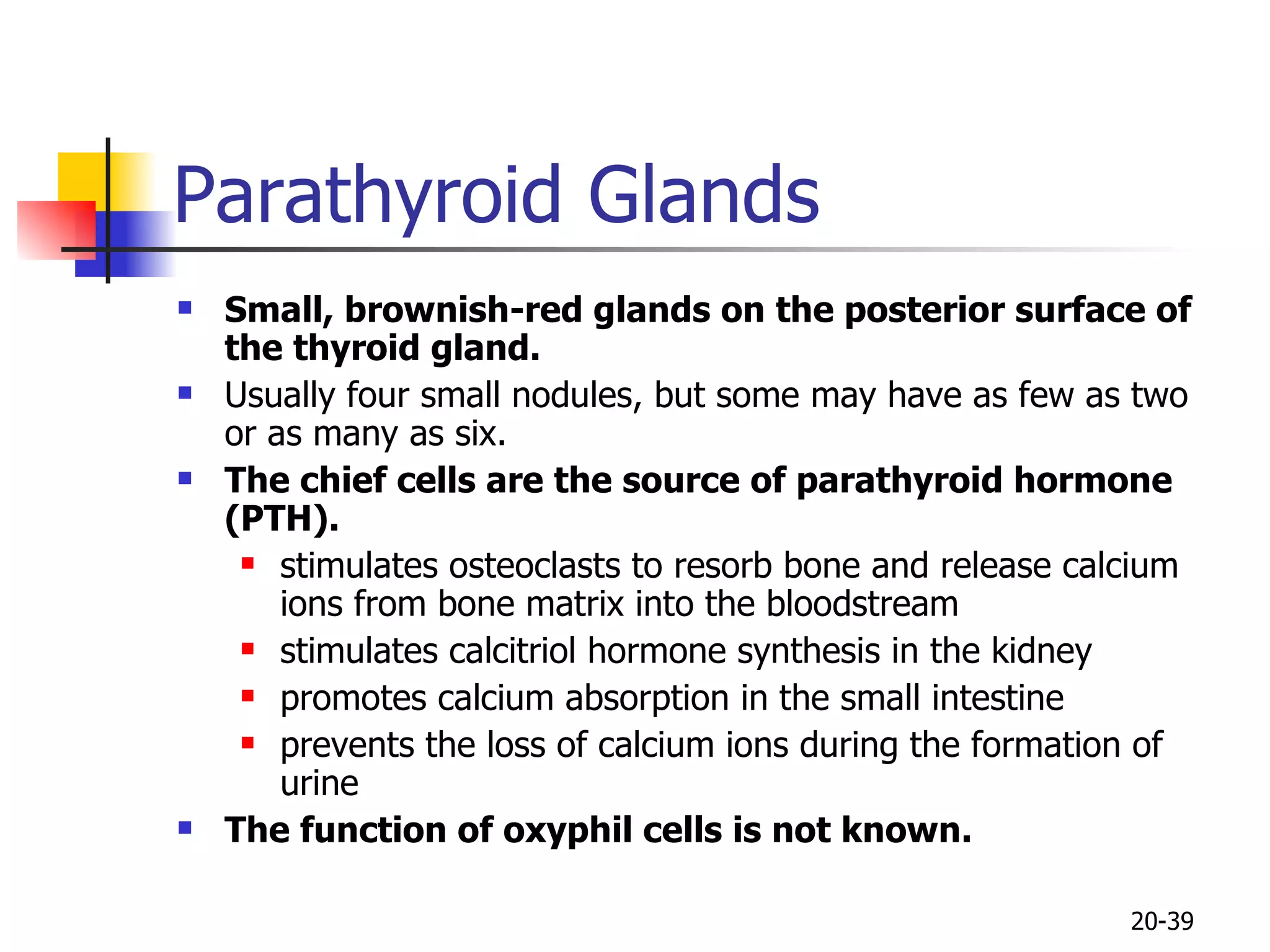
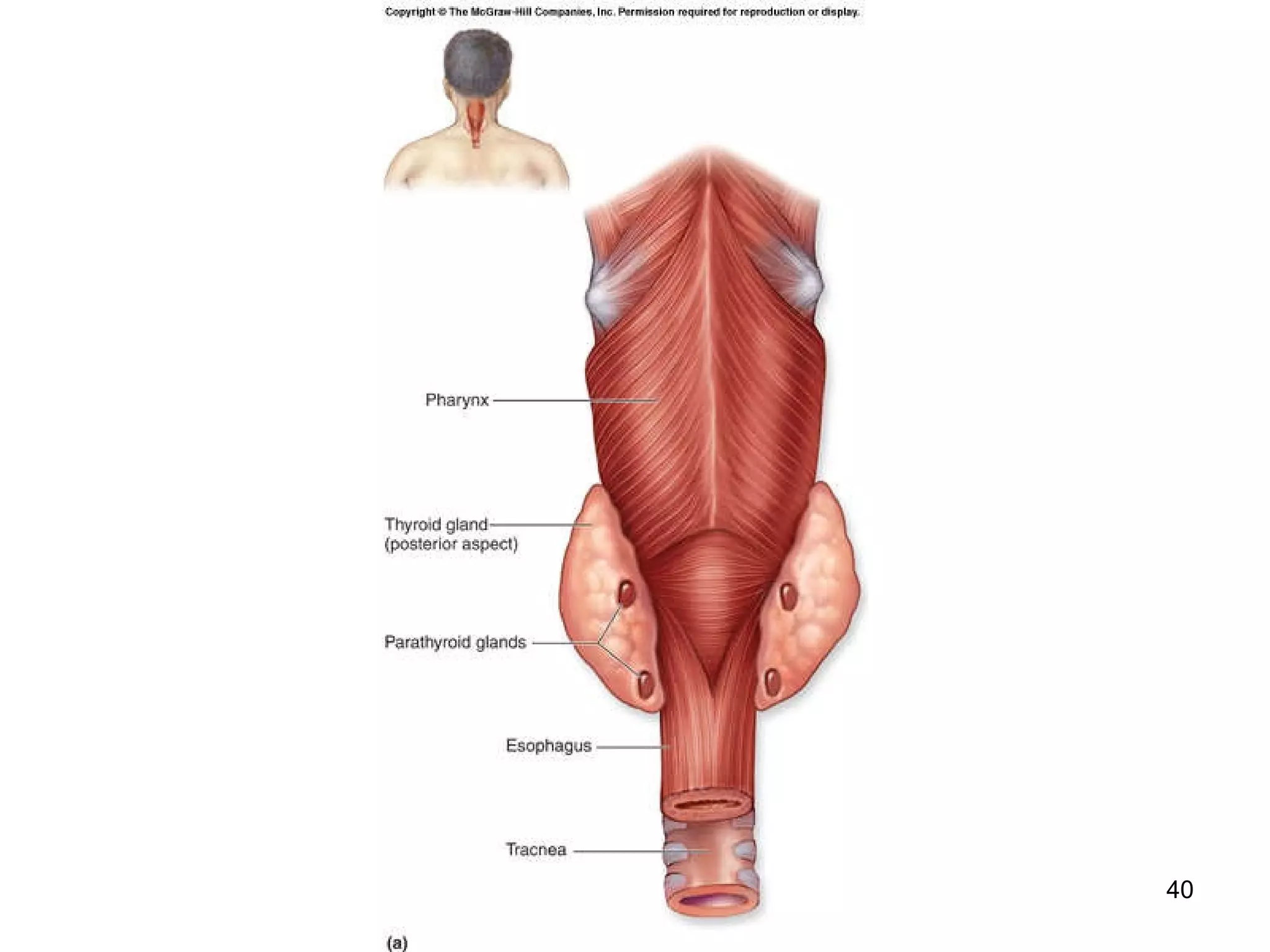
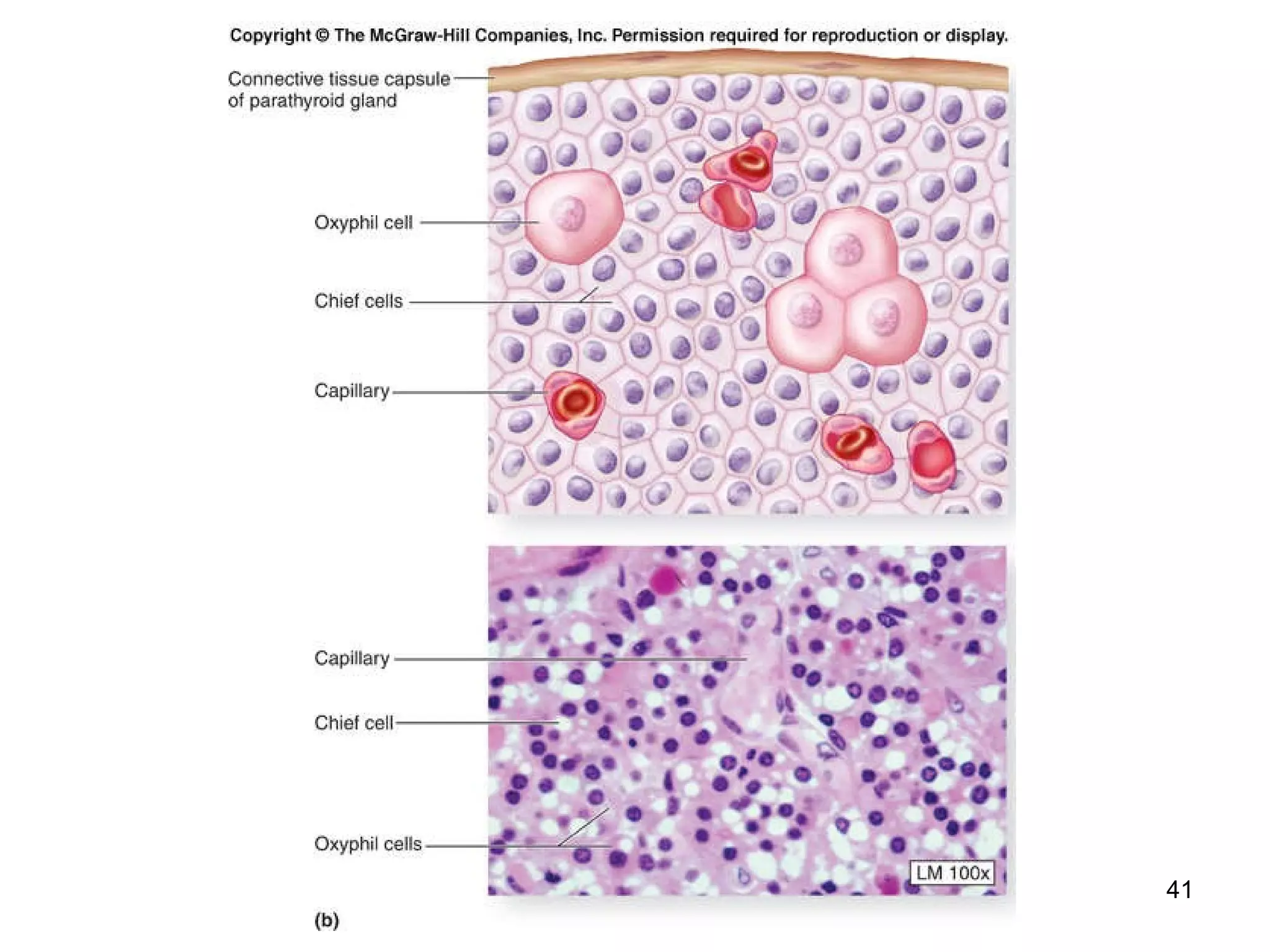
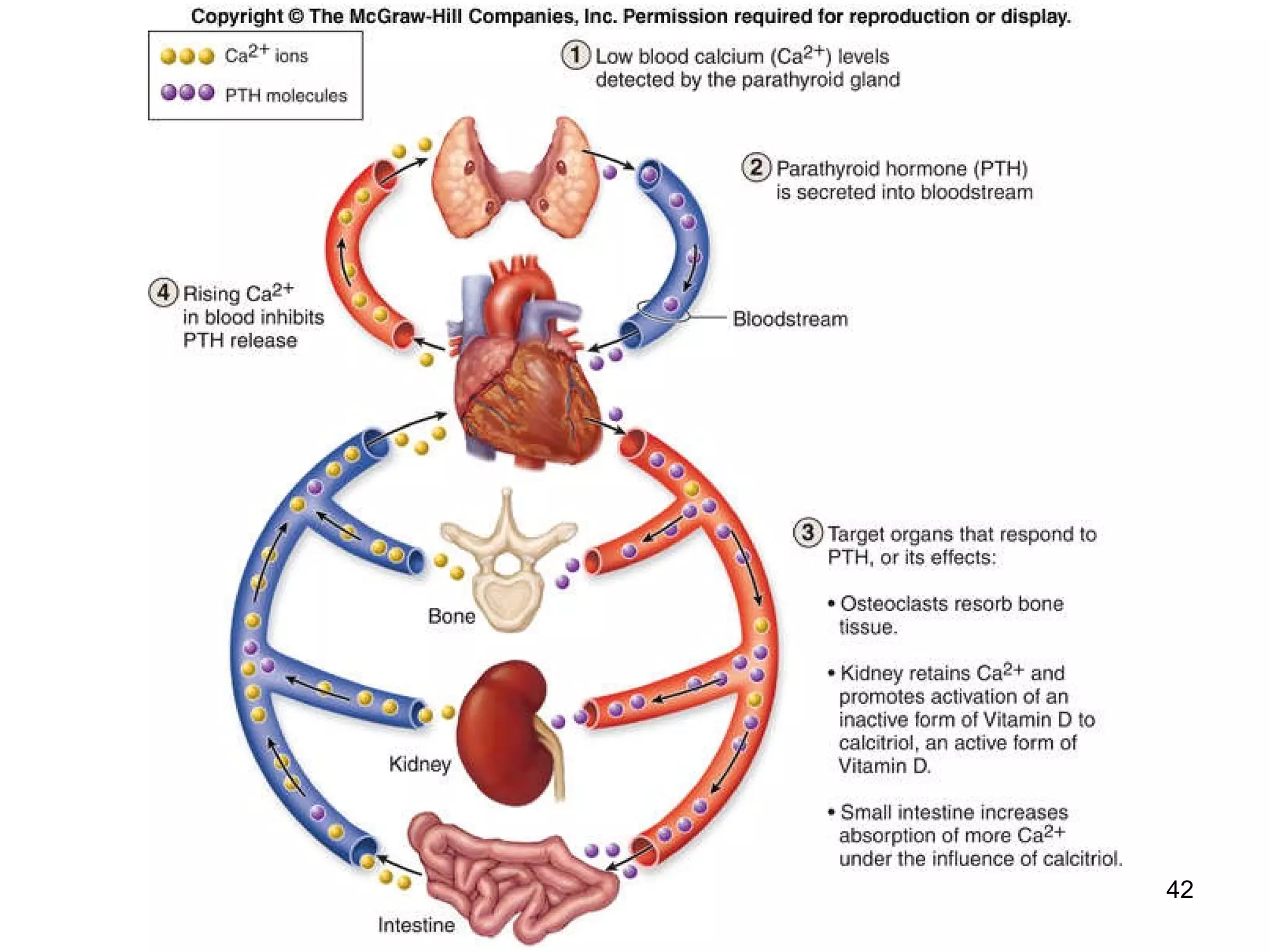
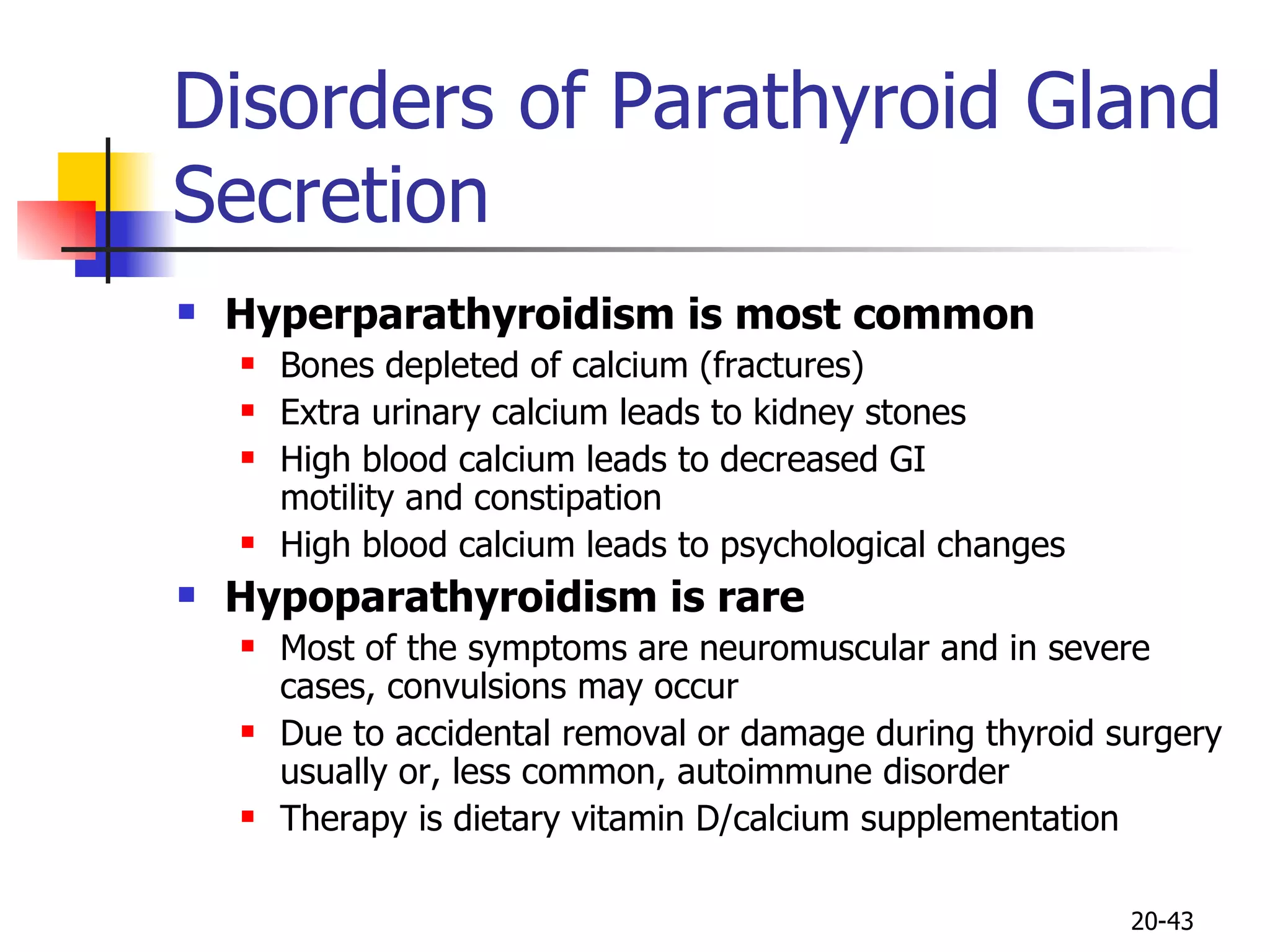
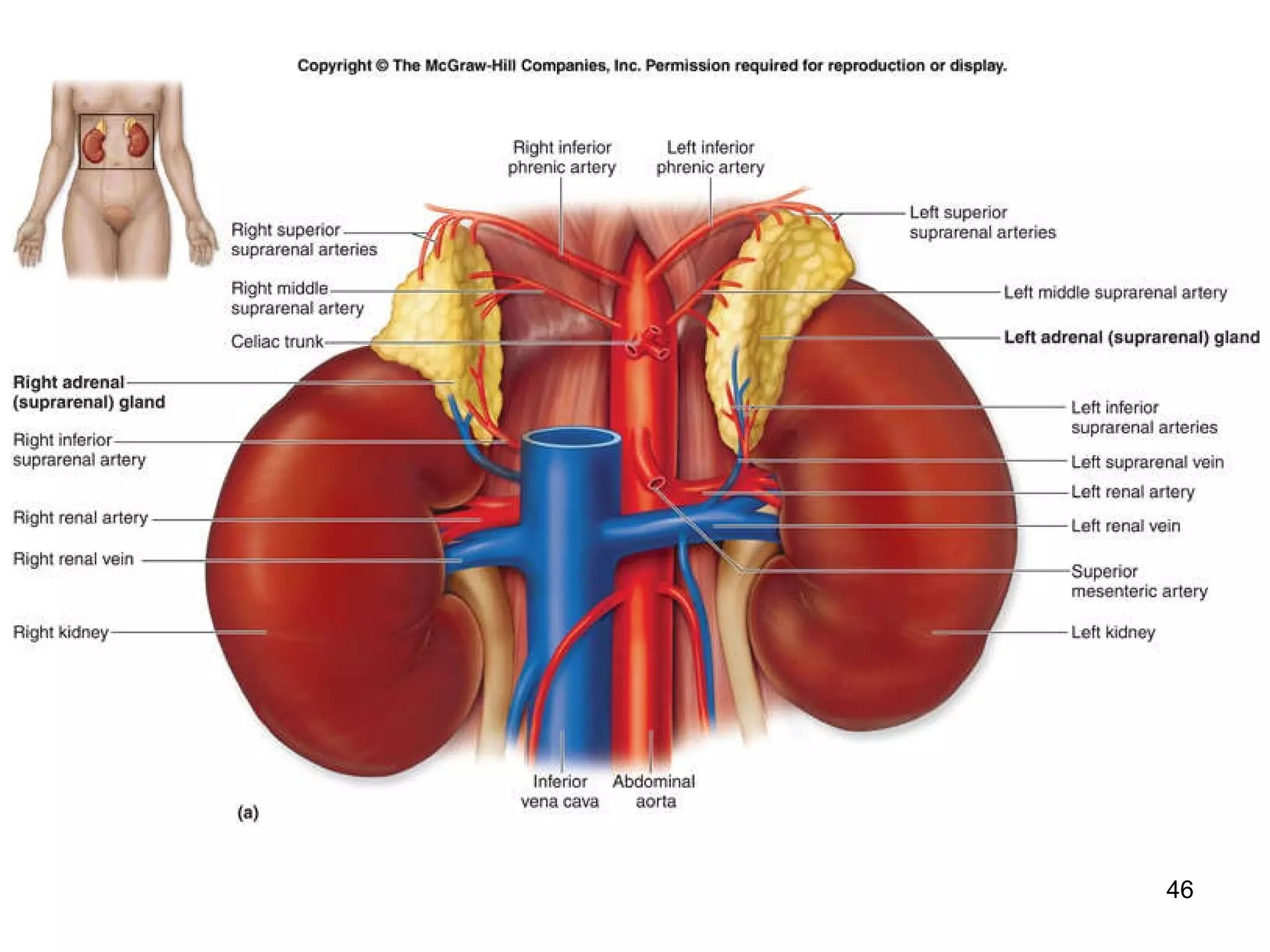
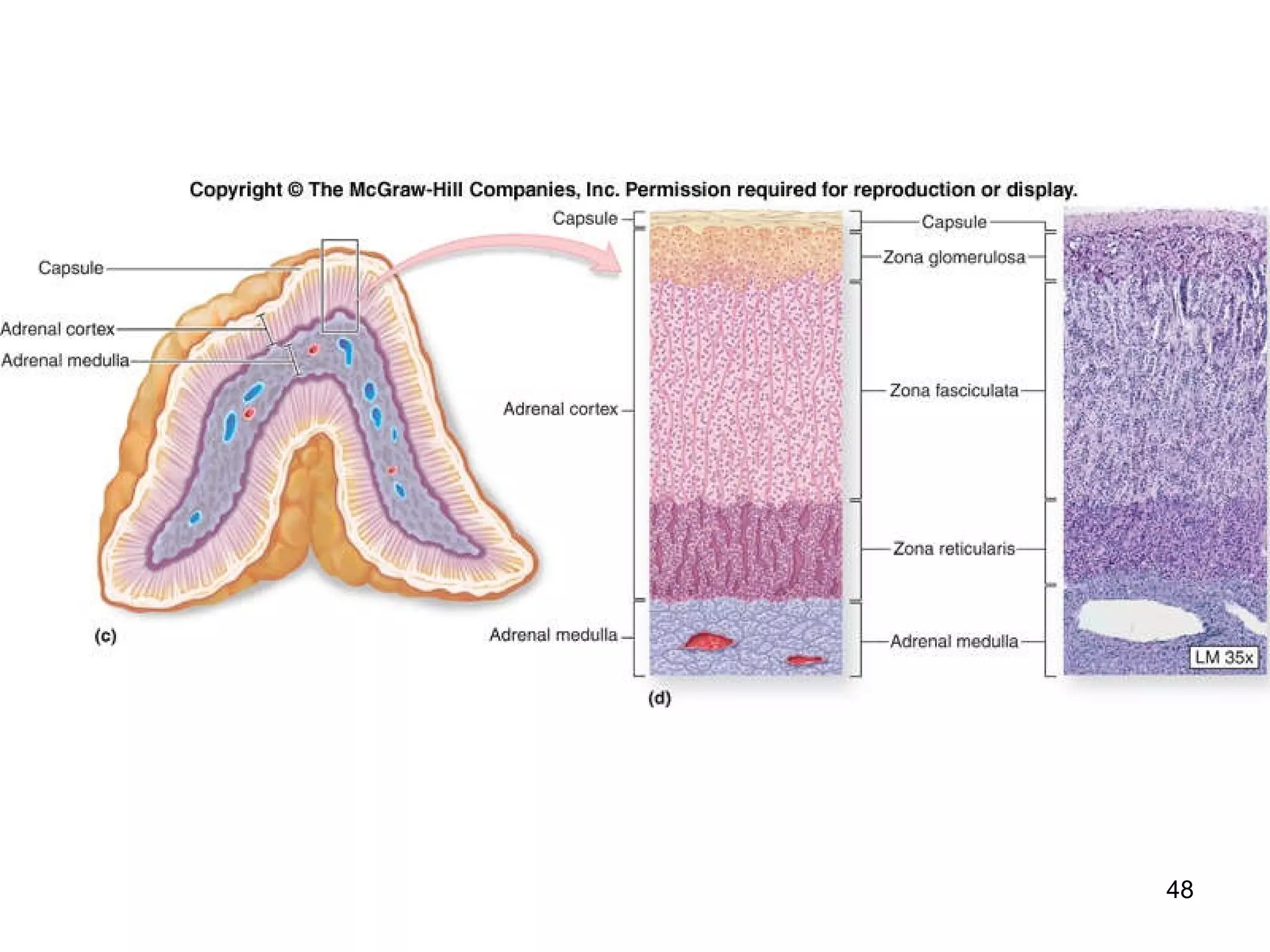
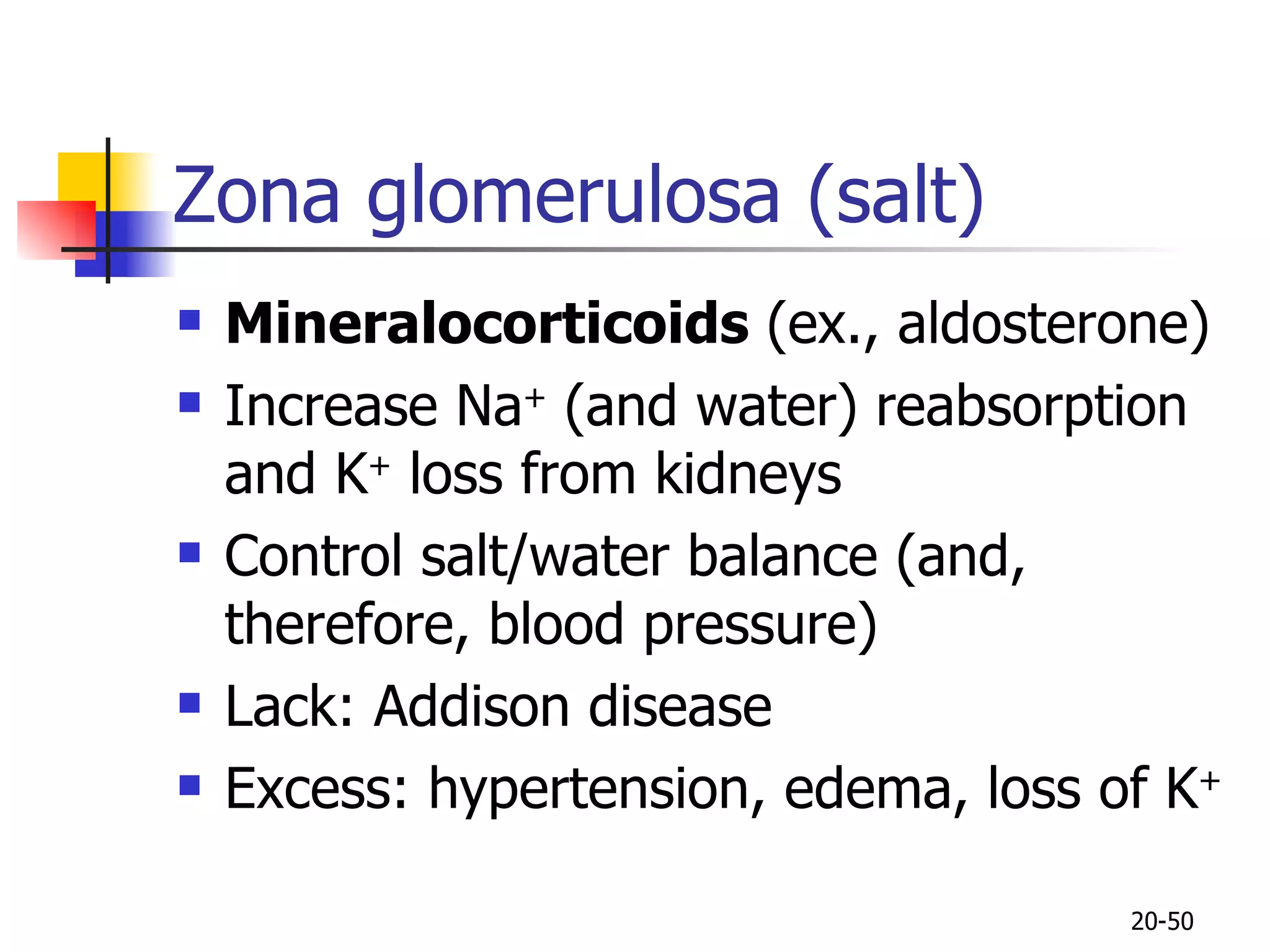
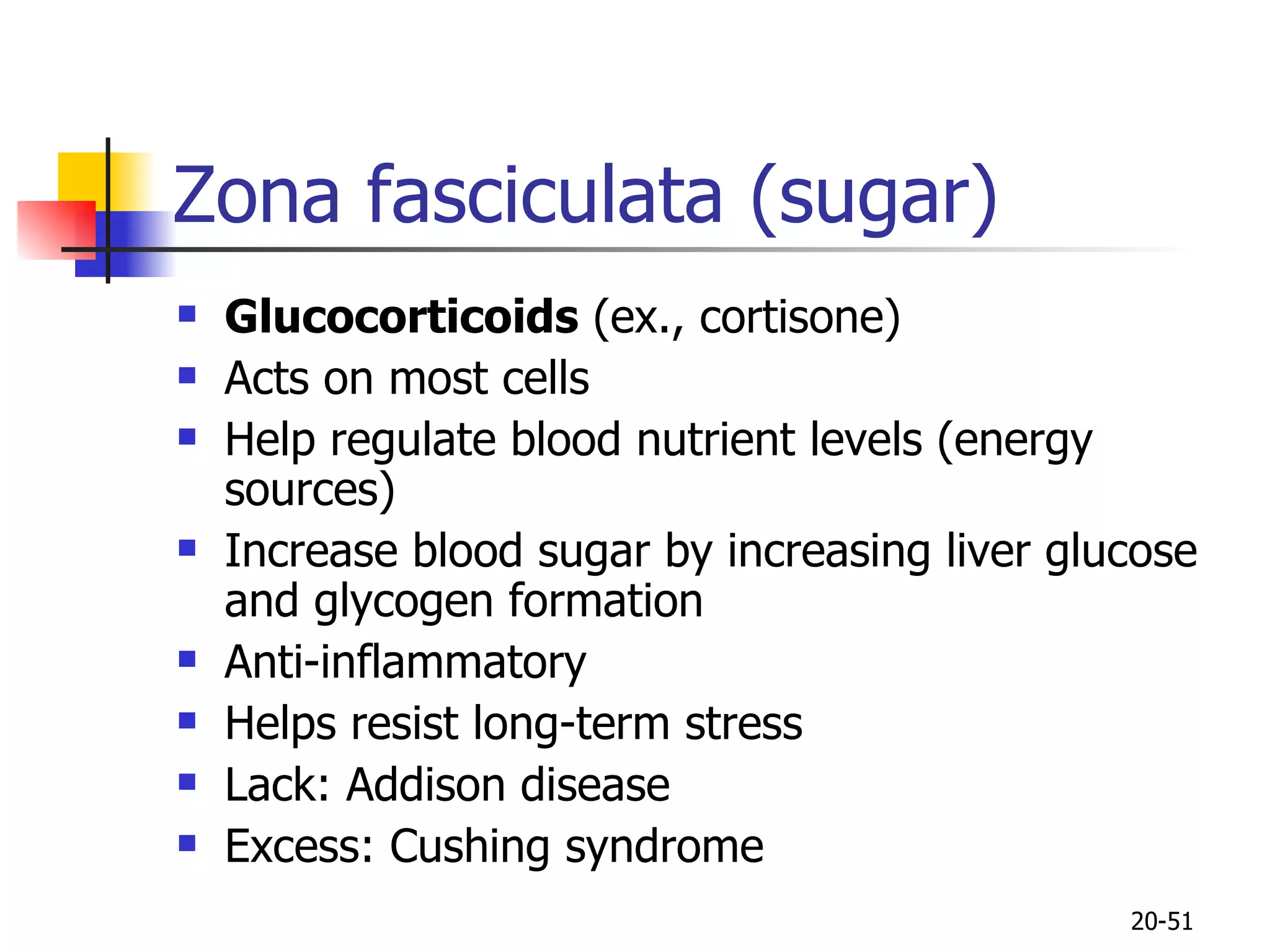
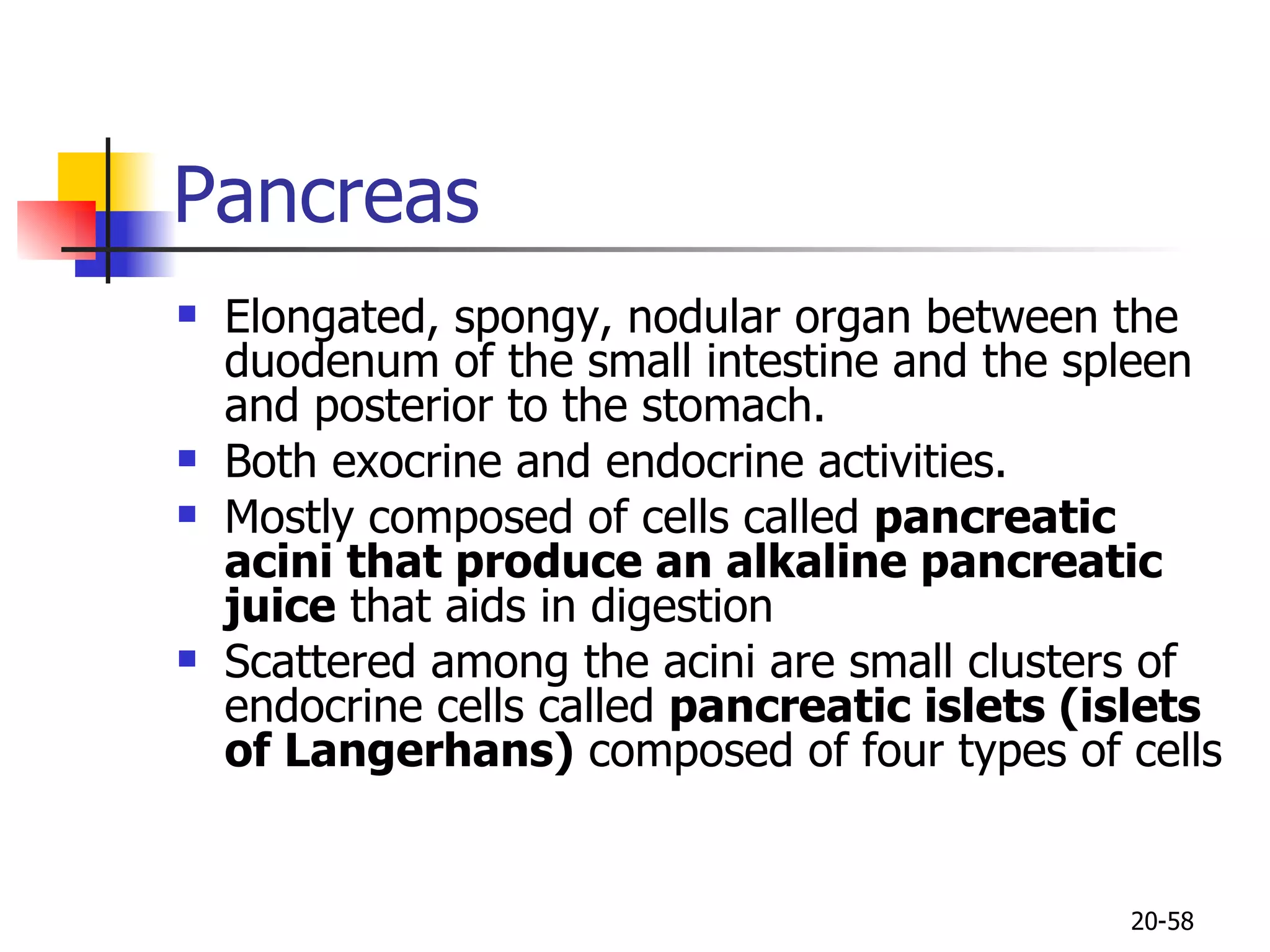
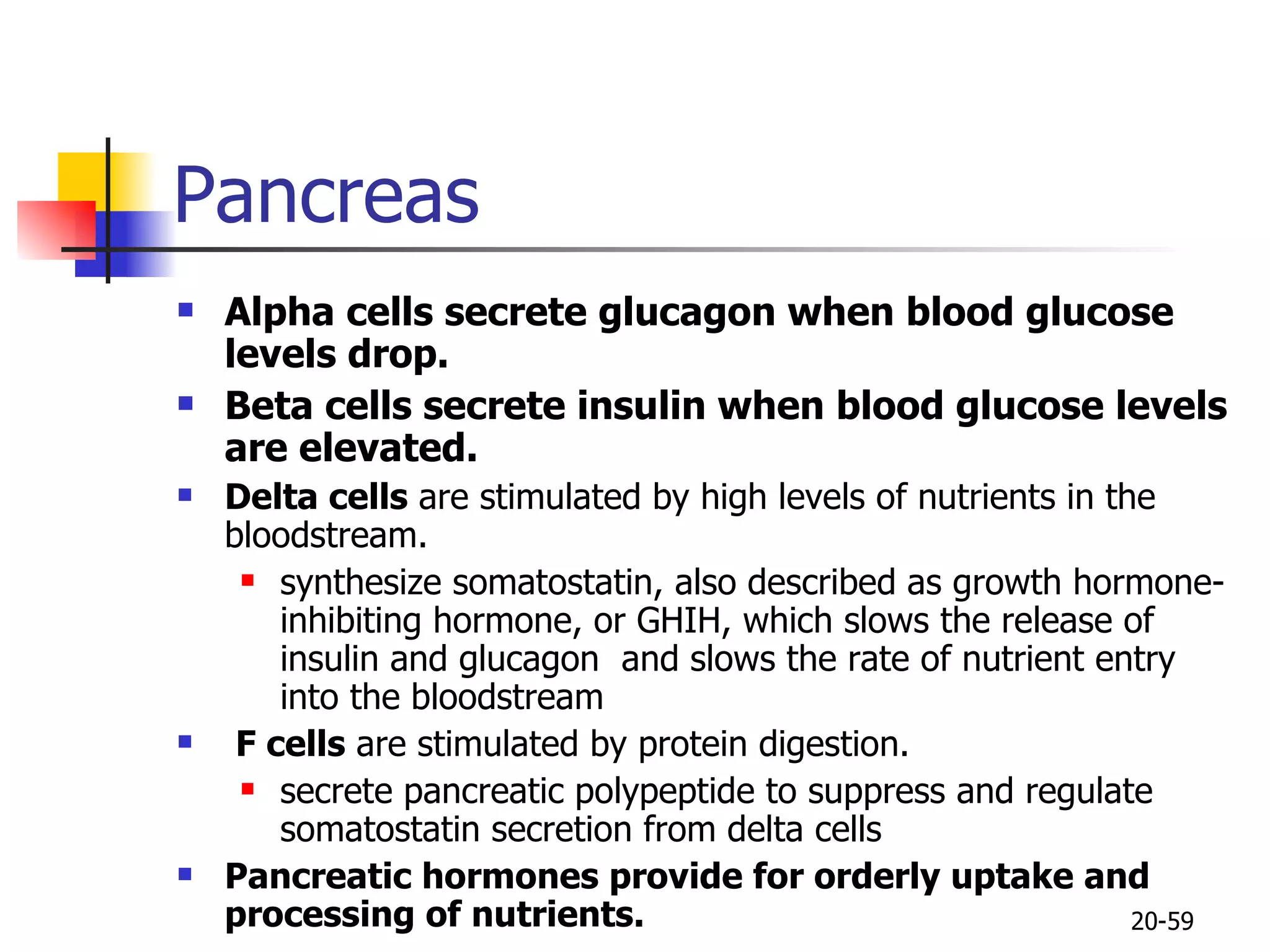
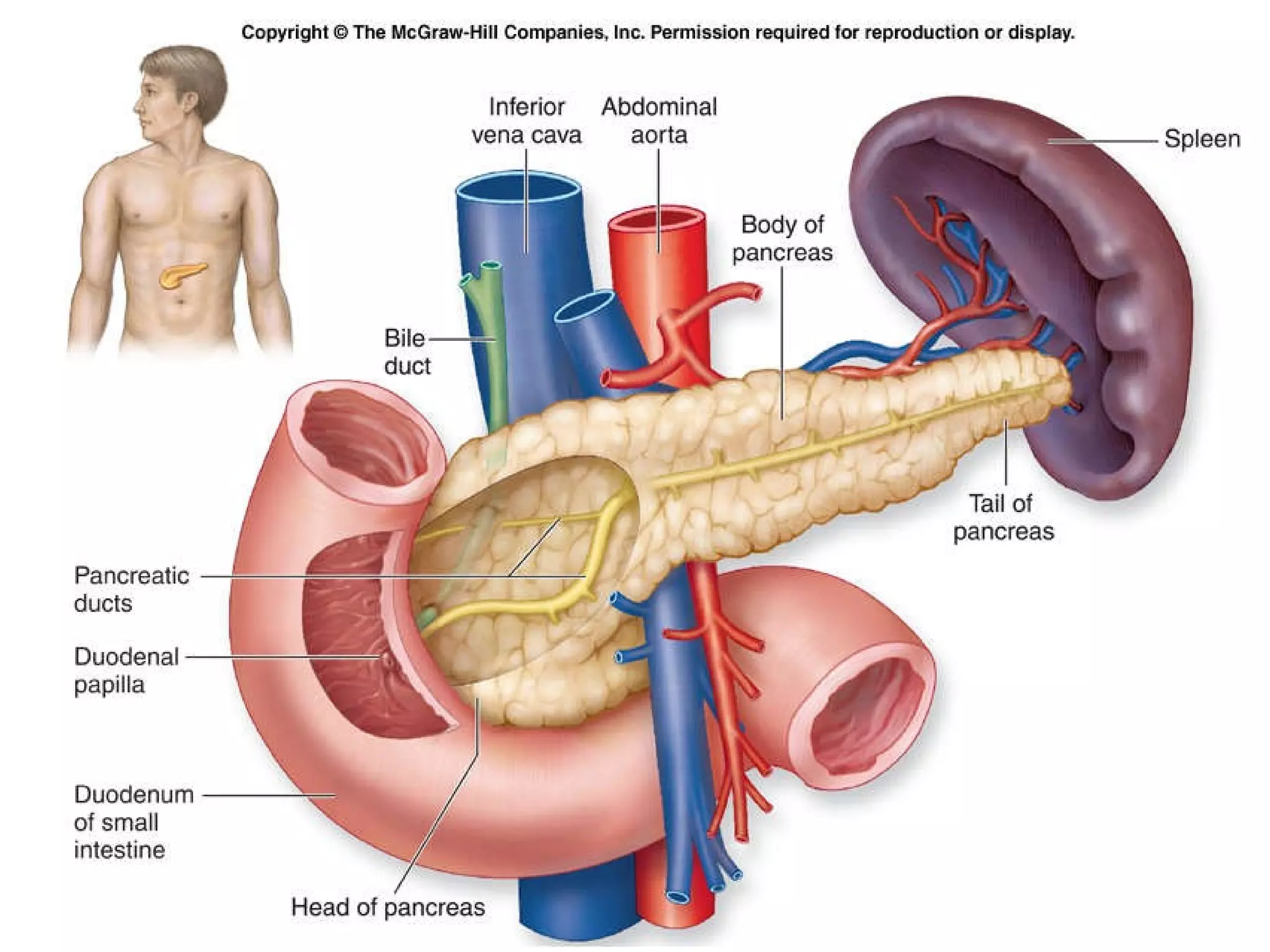
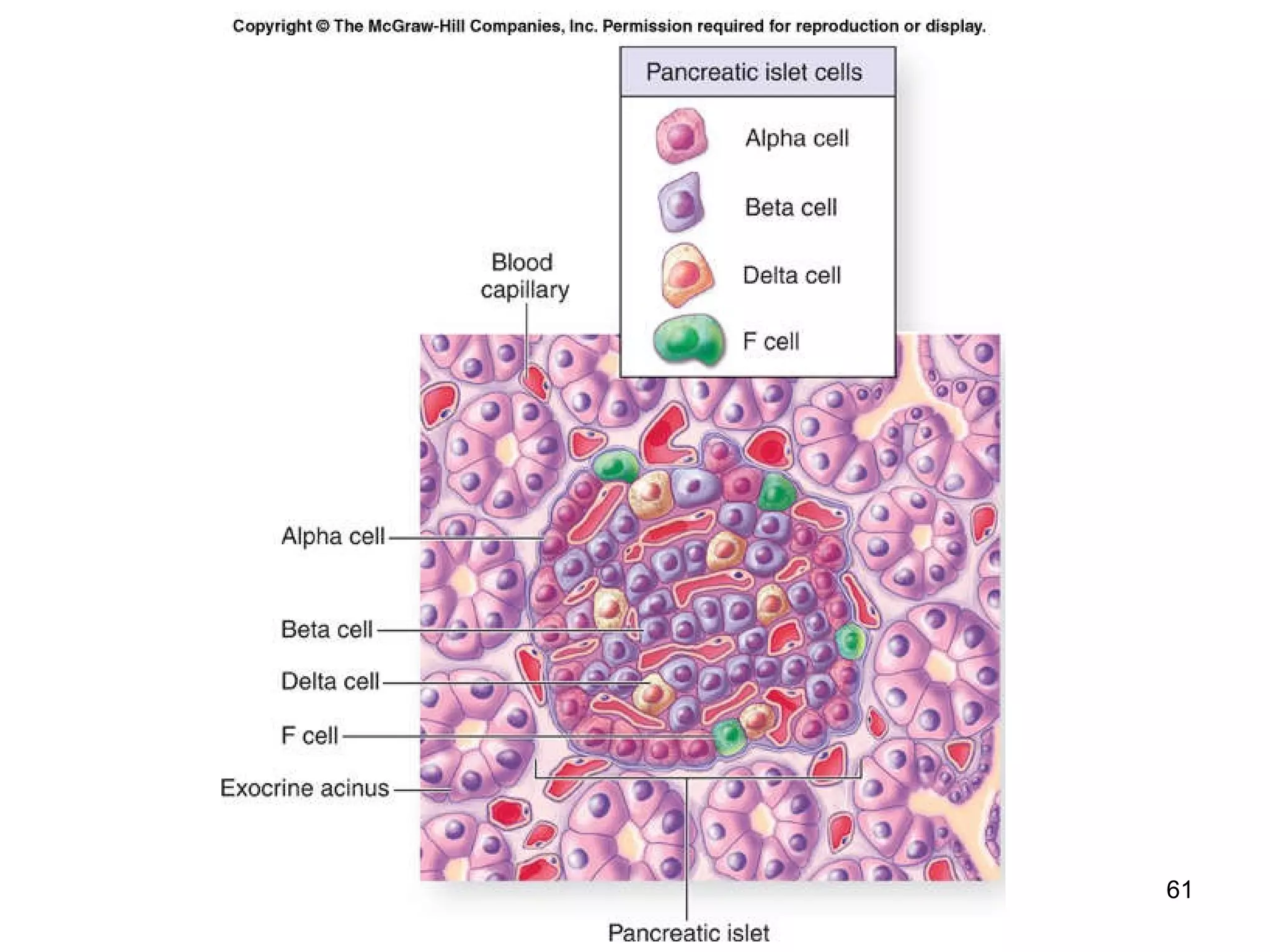
2) It describes the major endocrine glands and hormones, including the hypothalamus, pituitary gland, thyroid gland, parathyroid glands, and their functions.
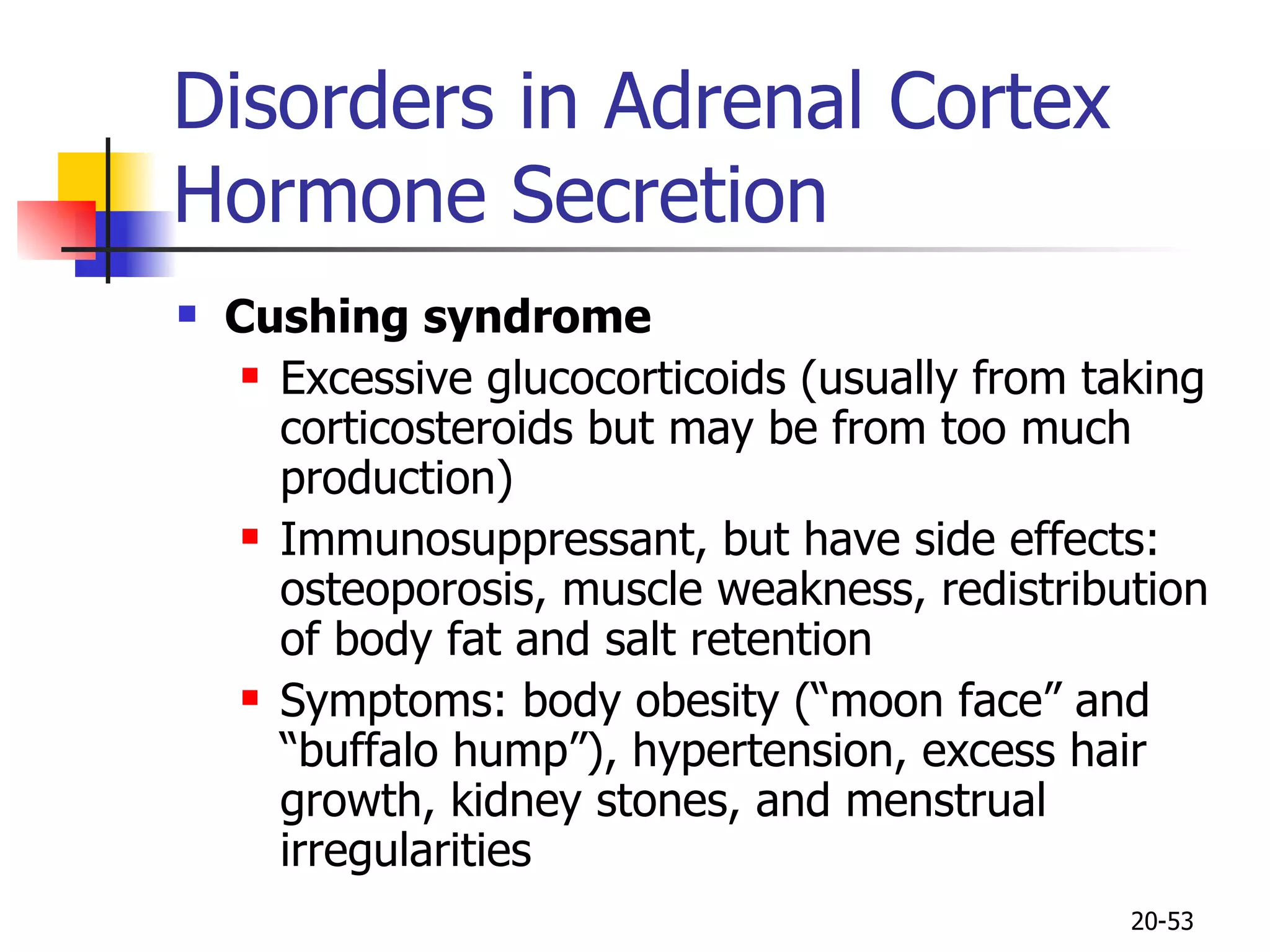
3) It explains disorders that can occur when endocrine gland secretions are abnormal, such as hyperthyroidism, hypothyroidism, and goiter.