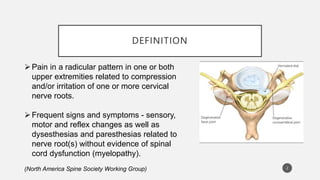
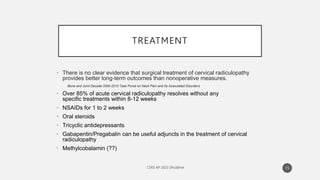
Cervical radiculopathy is pain caused by compression or irritation of cervical nerve roots. It commonly affects the C7 and C6 nerve roots and symptoms include pain and sensory or motor changes in the upper extremities. While most cases resolve within 3 months with conservative treatment like NSAIDs, oral steroids, or gabapentin, surgery may be considered for worsening symptoms. Minimally invasive posterior cervical foraminotomy has been shown to effectively treat radiculopathy with low complication rates and reduced need for further surgery compared to other options like anterior cervical discectomy and fusion.