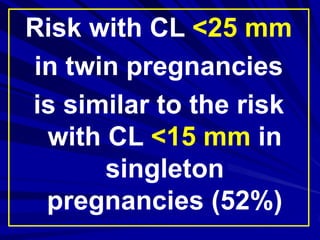
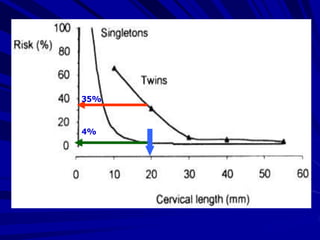
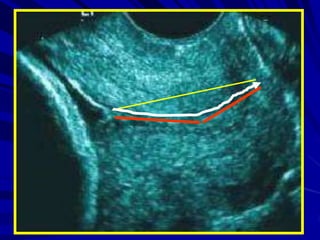
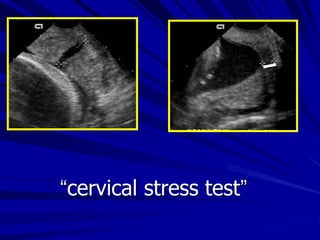
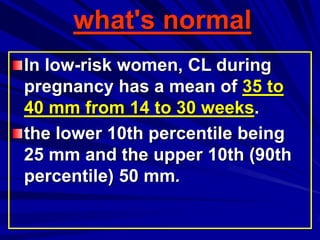
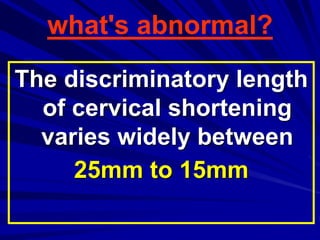
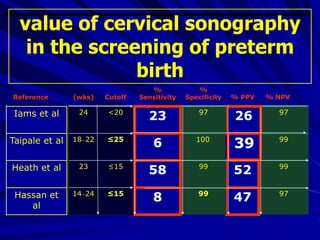
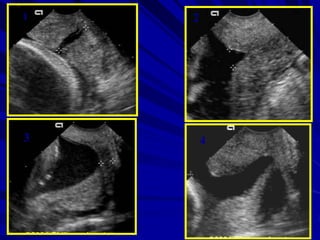
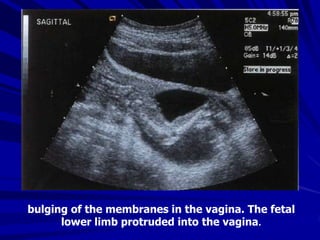
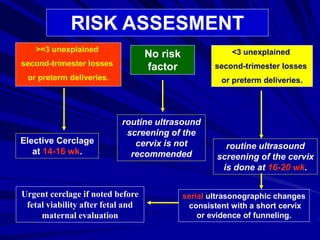
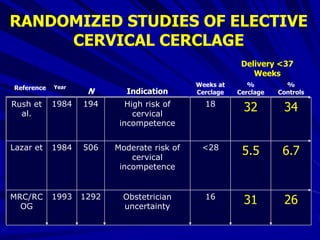
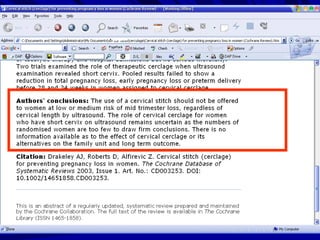
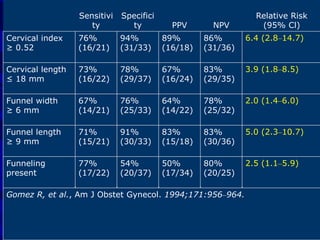
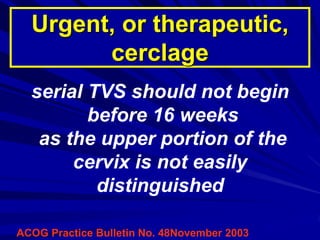
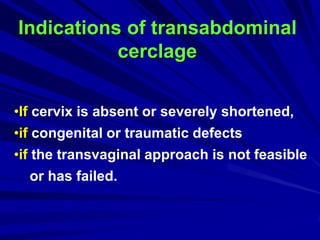
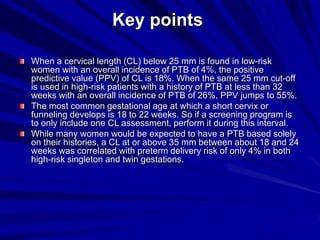
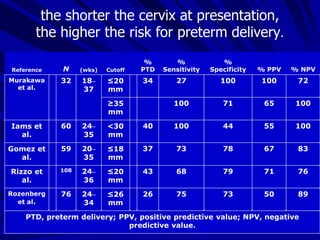
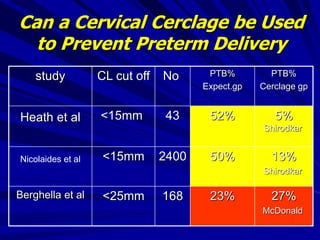
Ultrasonographic screening of the cervix can help predict preterm birth risk but has limitations. A cervical length below 25mm has low predictive value in low-risk women but higher value in high-risk groups. Screening is best done between 16-22 weeks as most cervical changes occur then. Therapeutic cerclage for progressive cervical shortening or funneling may help prevent preterm delivery but randomized trials have had mixed results. Transabdominal cerclage is an alternative for women with prior failed vaginal cerclages or cervical abnormalities.