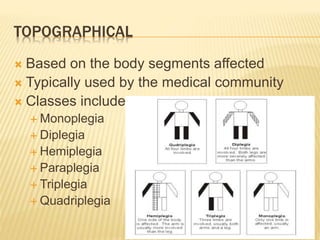
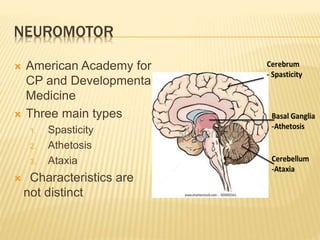
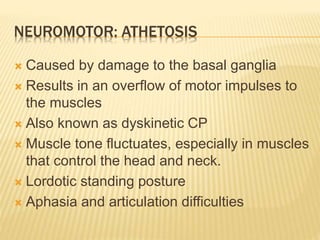
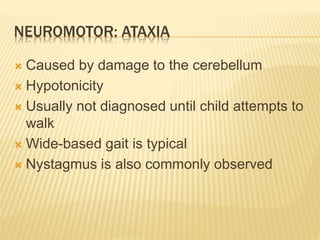
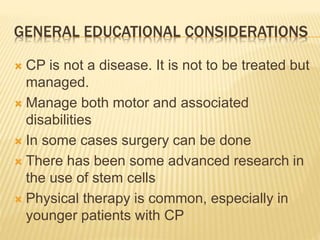
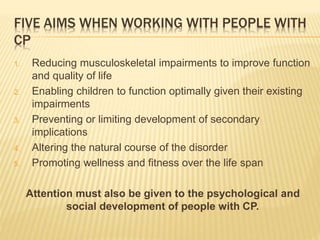
This document discusses cerebral palsy (CP), a group of permanent disorders caused by damage to the developing brain that affects body movement and muscle tone. CP symptoms can range from mild to severe and vary depending on the location and degree of brain damage. It is classified in different ways including by the affected body parts (topographical), type of movement abnormality (neuromotor), and functional ability. While CP is non-progressive, physical therapy and management of symptoms can help reduce impairments and secondary complications over the lifespan.