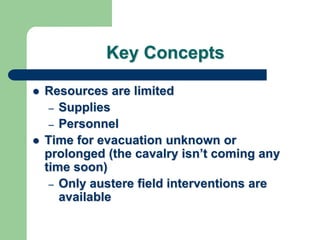
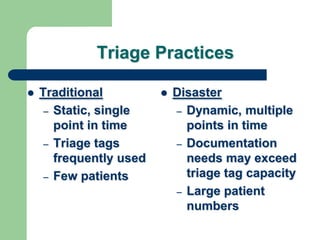
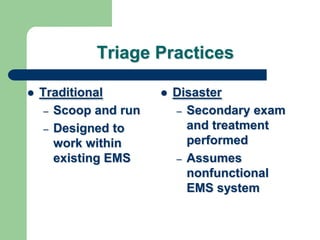
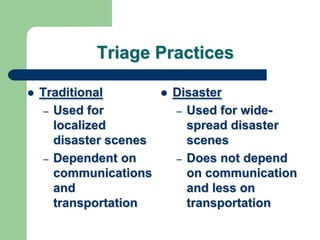
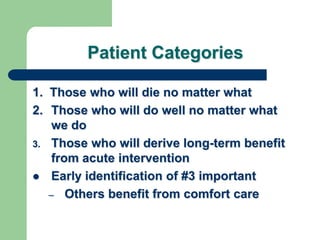
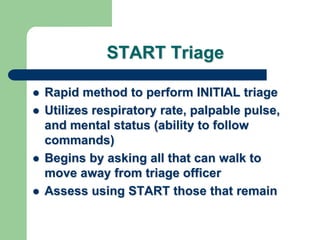
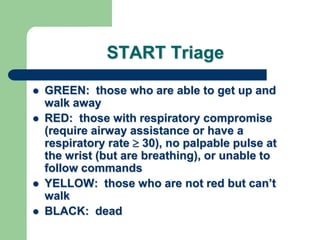
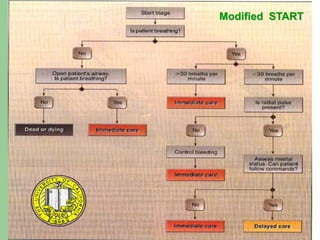
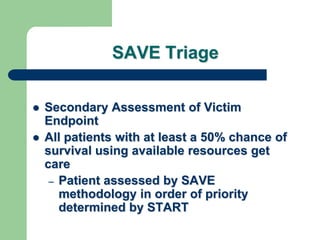
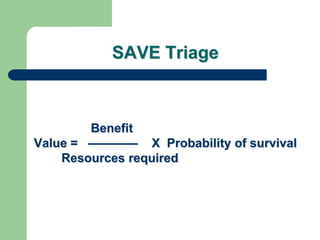
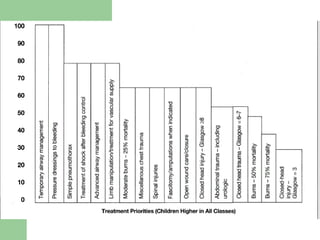
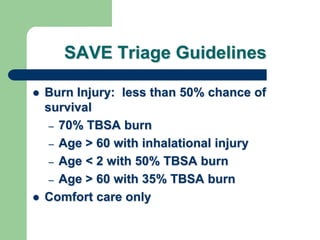
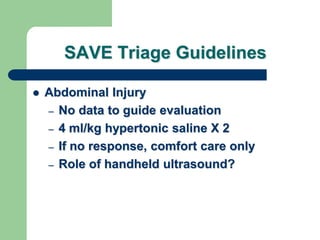
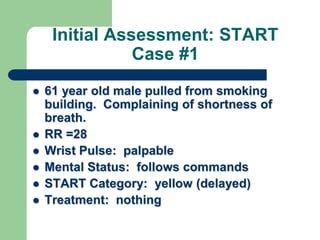
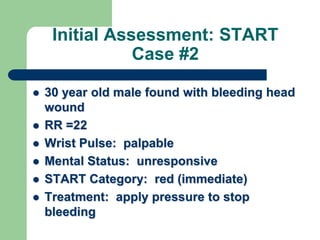
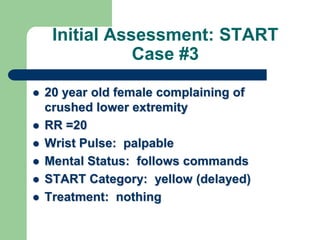
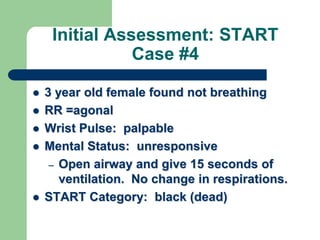
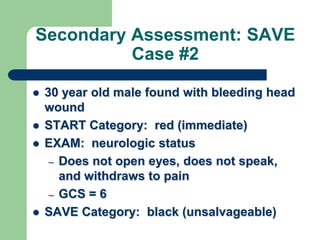
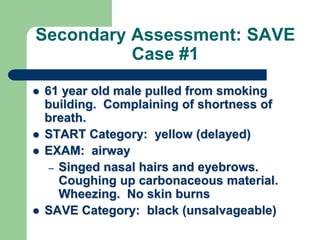
1) The document discusses disaster triage methods START and SAVE which are used to prioritize patients with limited resources. START uses respiratory rate, pulse, and mental status to categorize patients as red, yellow, black. SAVE provides a more thorough secondary exam of red-tagged patients.
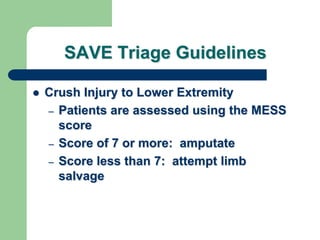
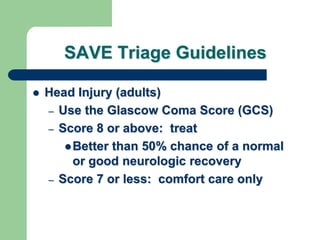
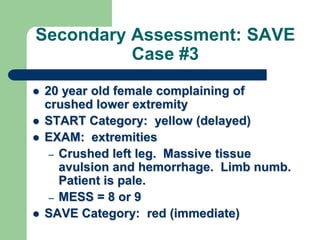
2) A case example demonstrates START and SAVE triage in action. A head injury patient is initially red-tagged but deemed unsalvageable on secondary exam due to low GCS. A shortness of breath patient is found to have inhalation injuries and is deemed unsalvageable. A crushed leg patient is red-tagged and prioritized for immediate intervention.