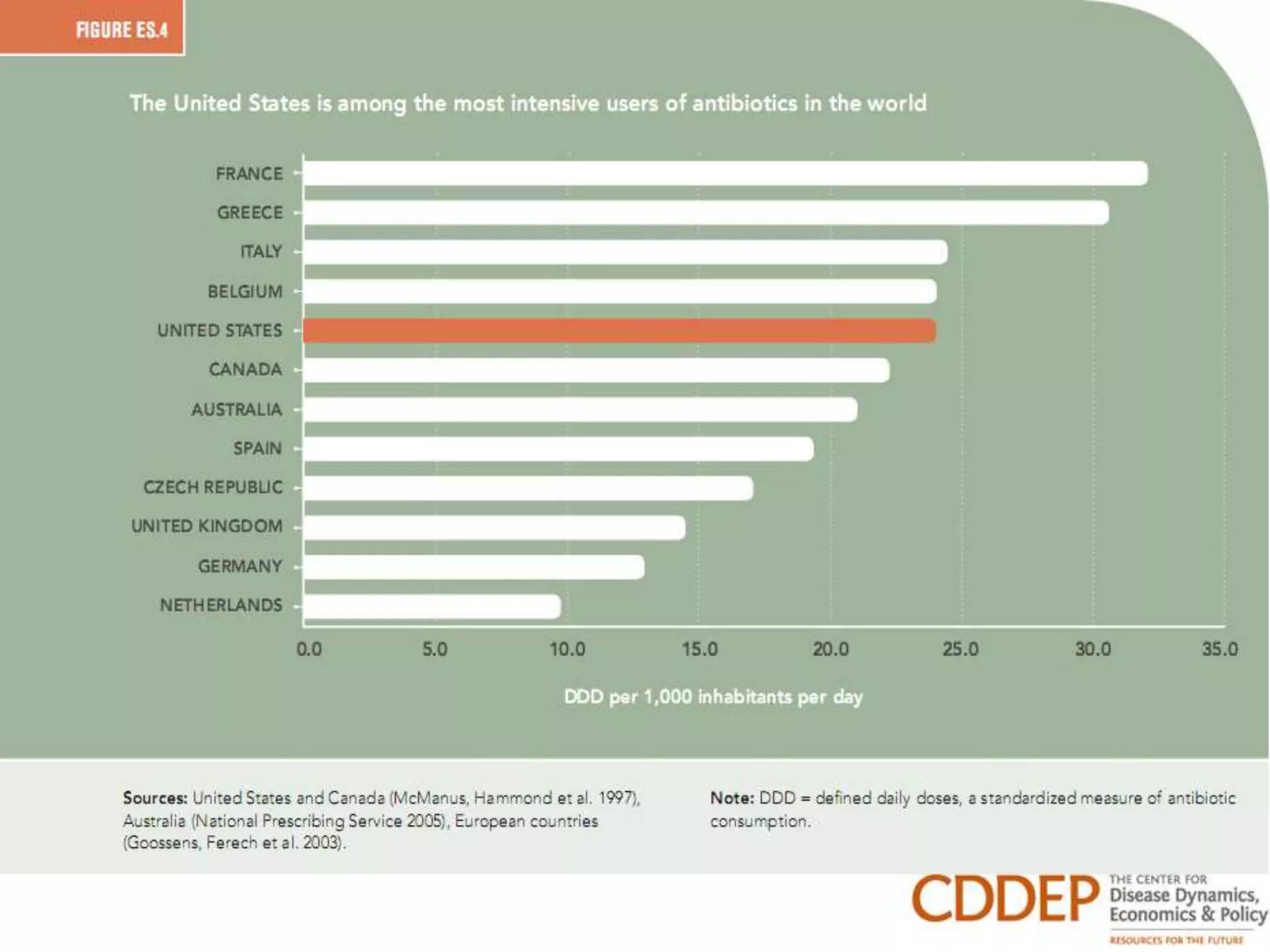
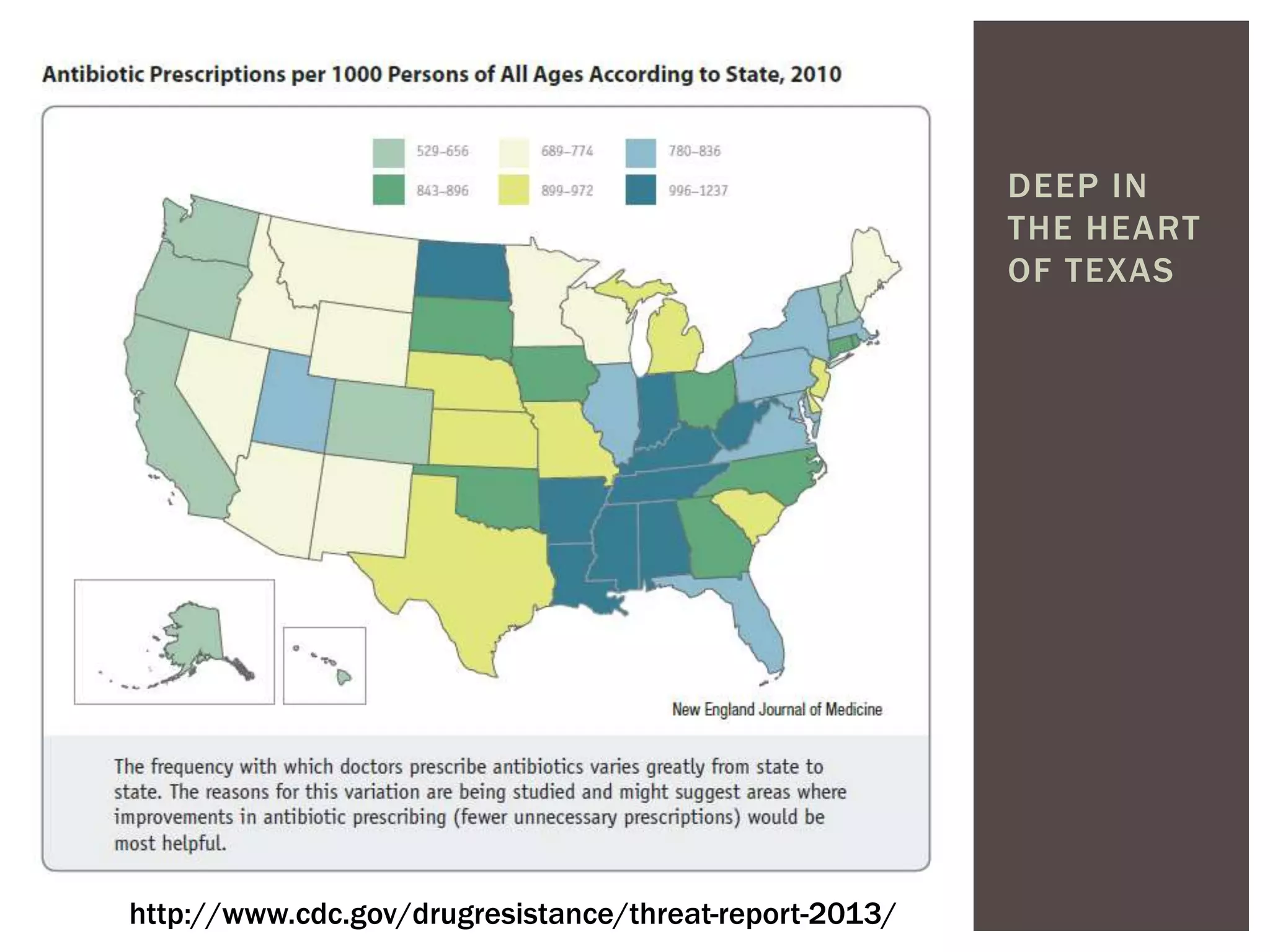
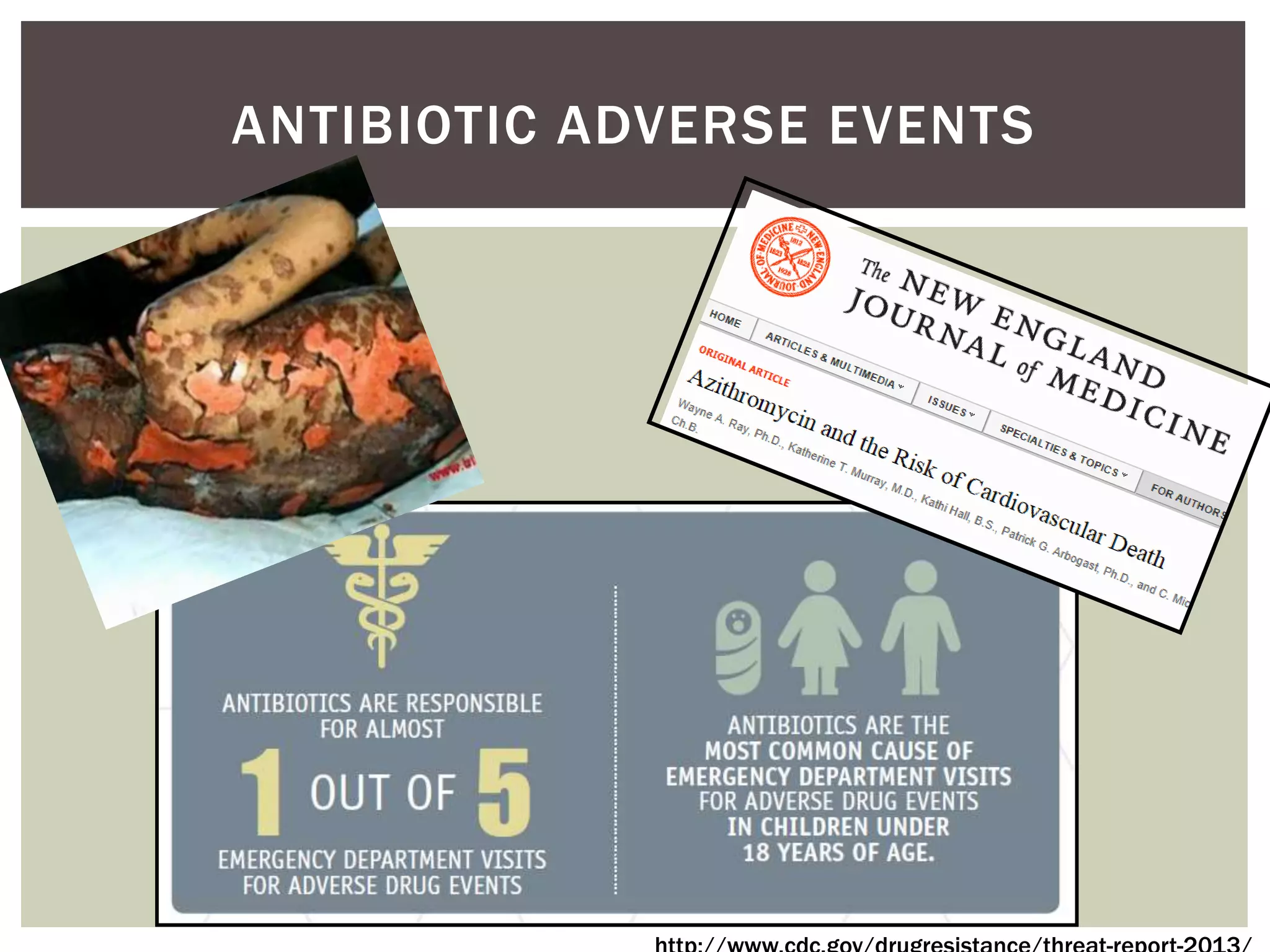
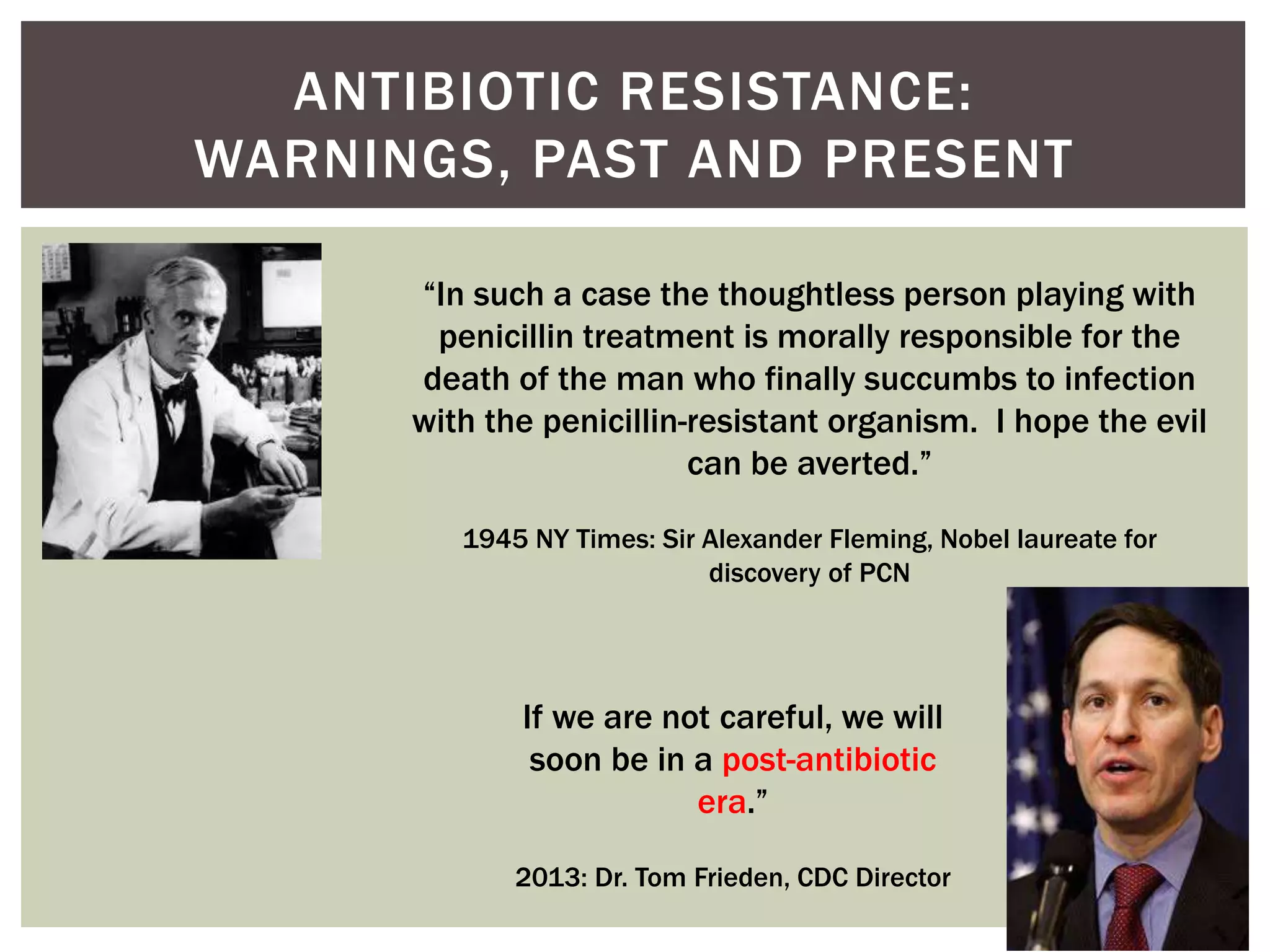
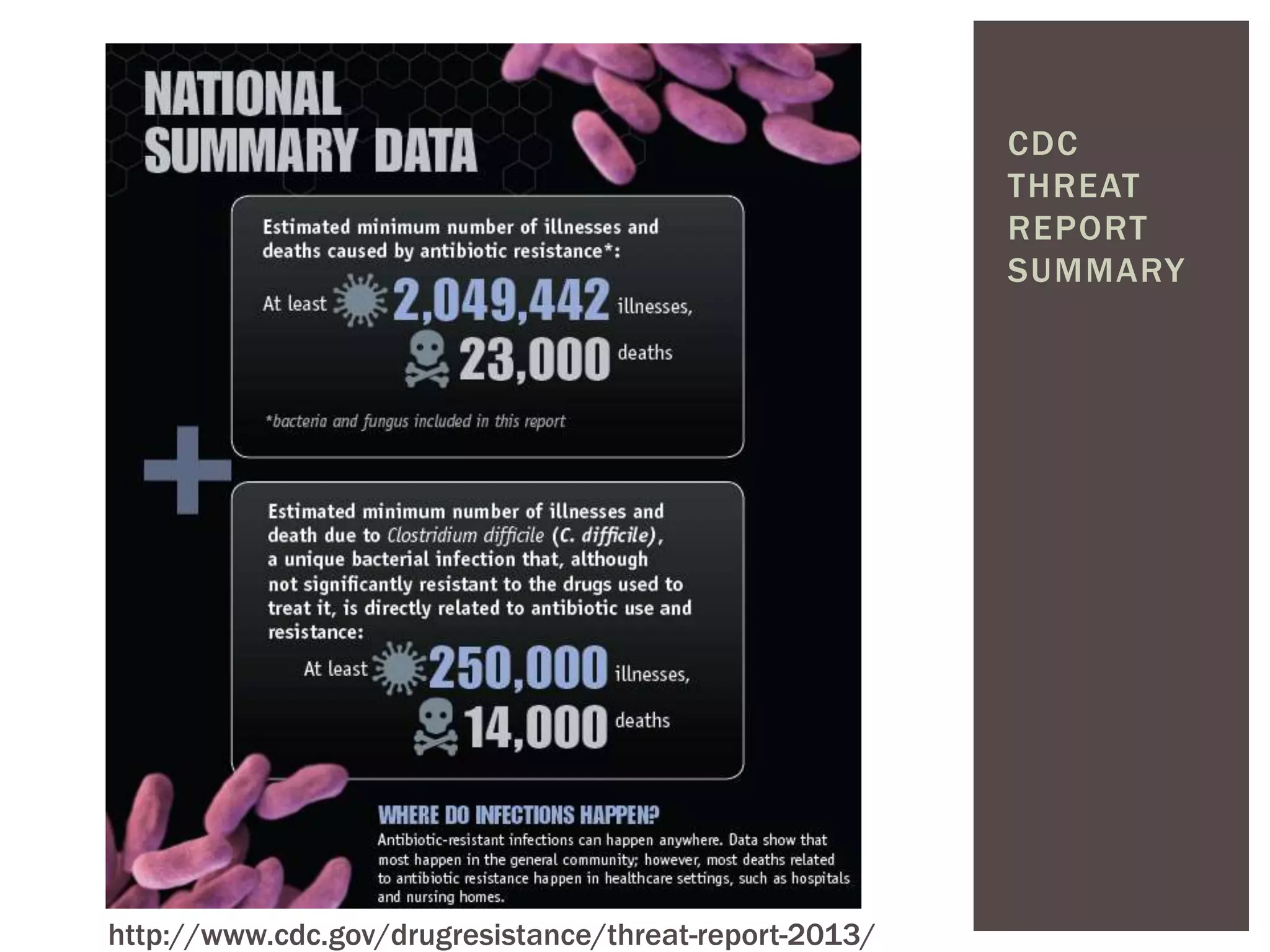
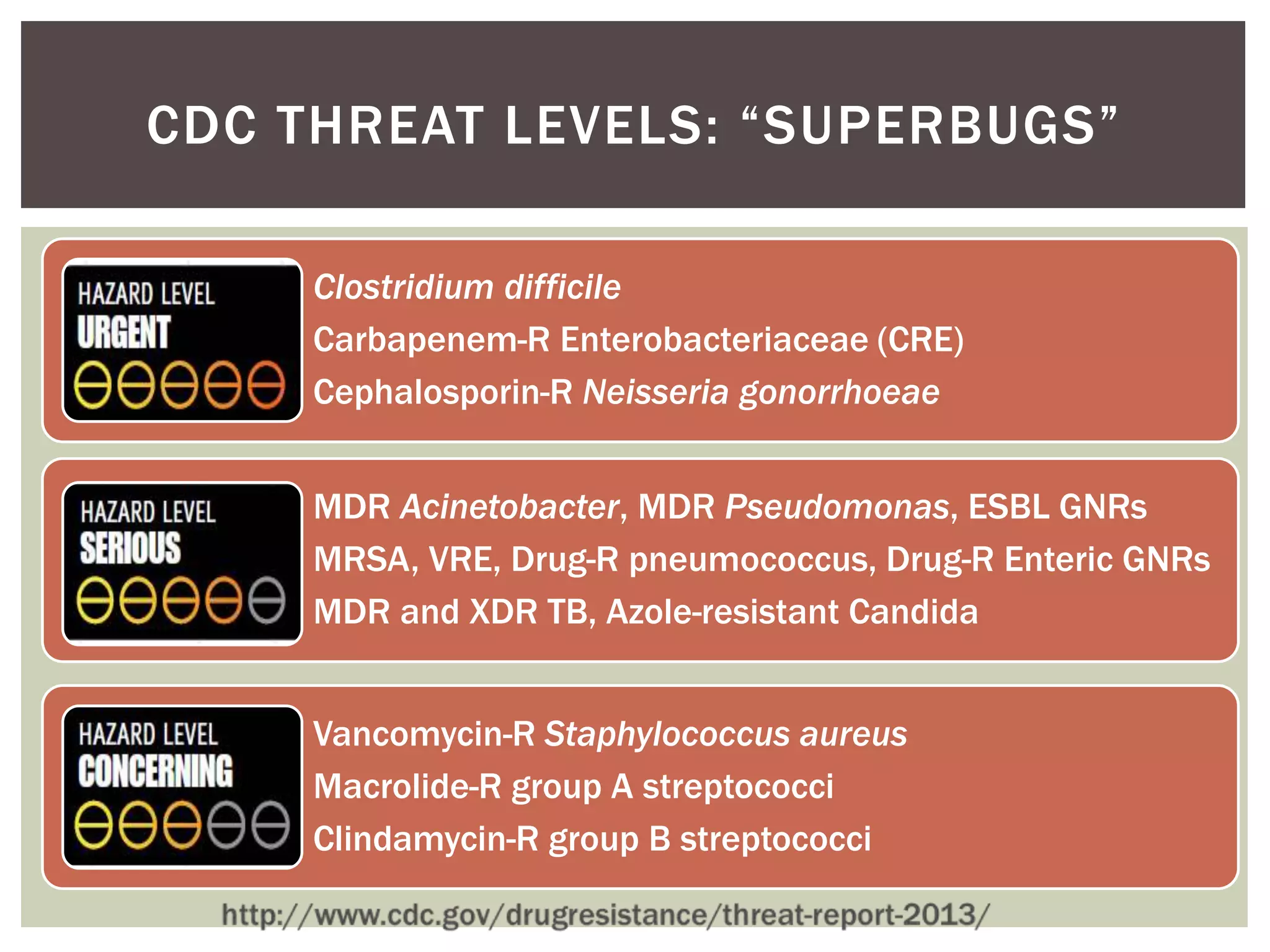
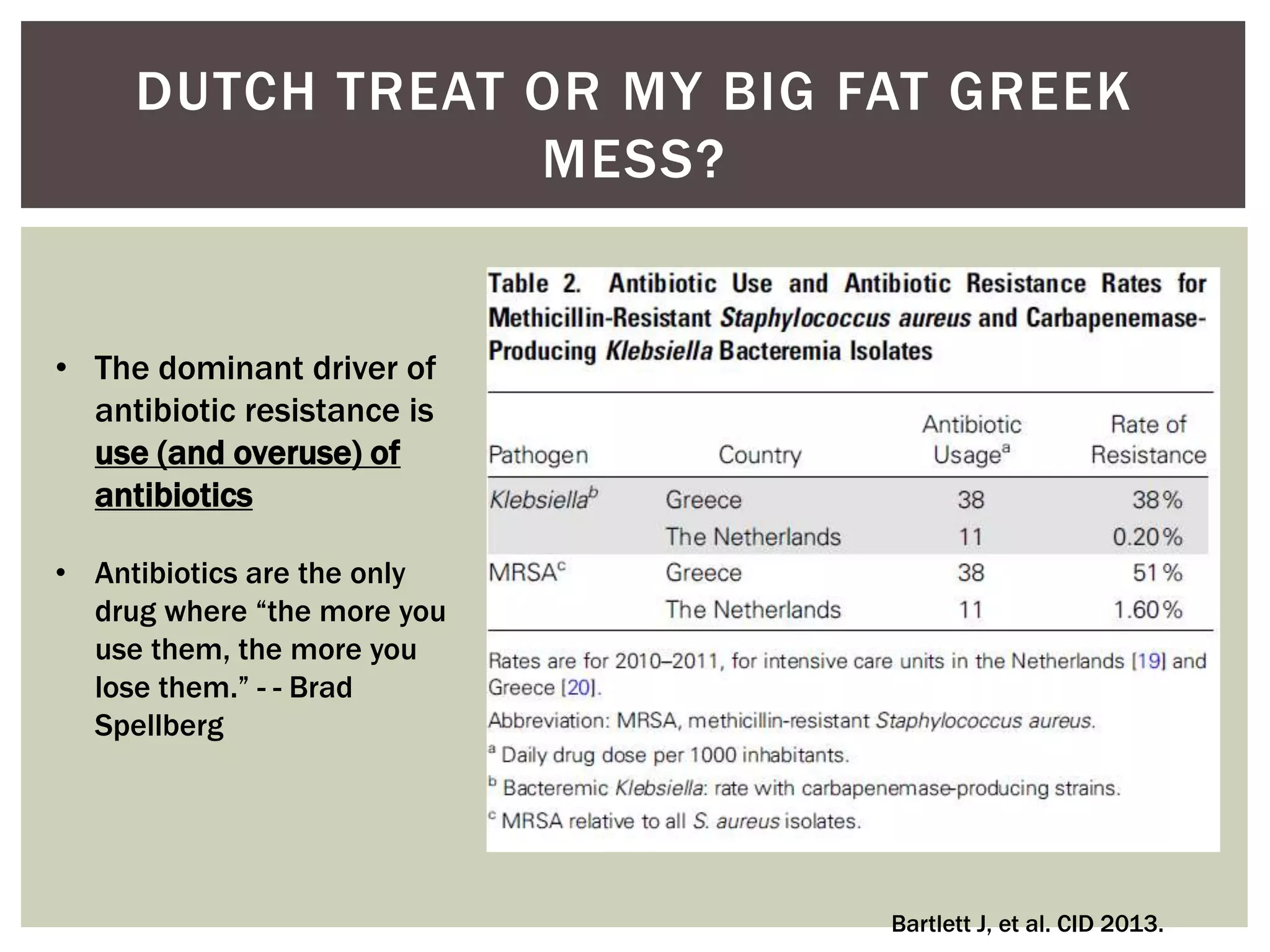
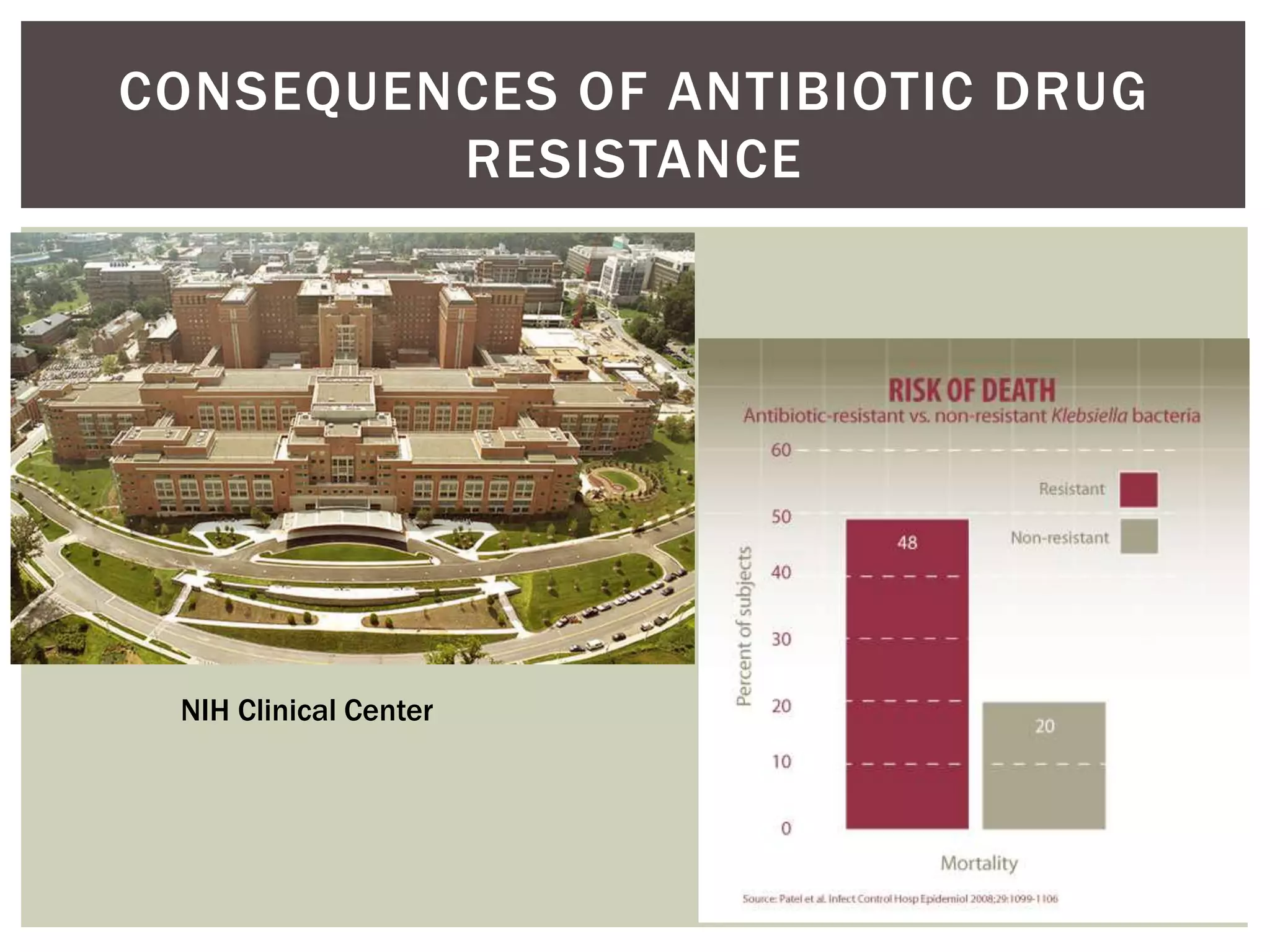
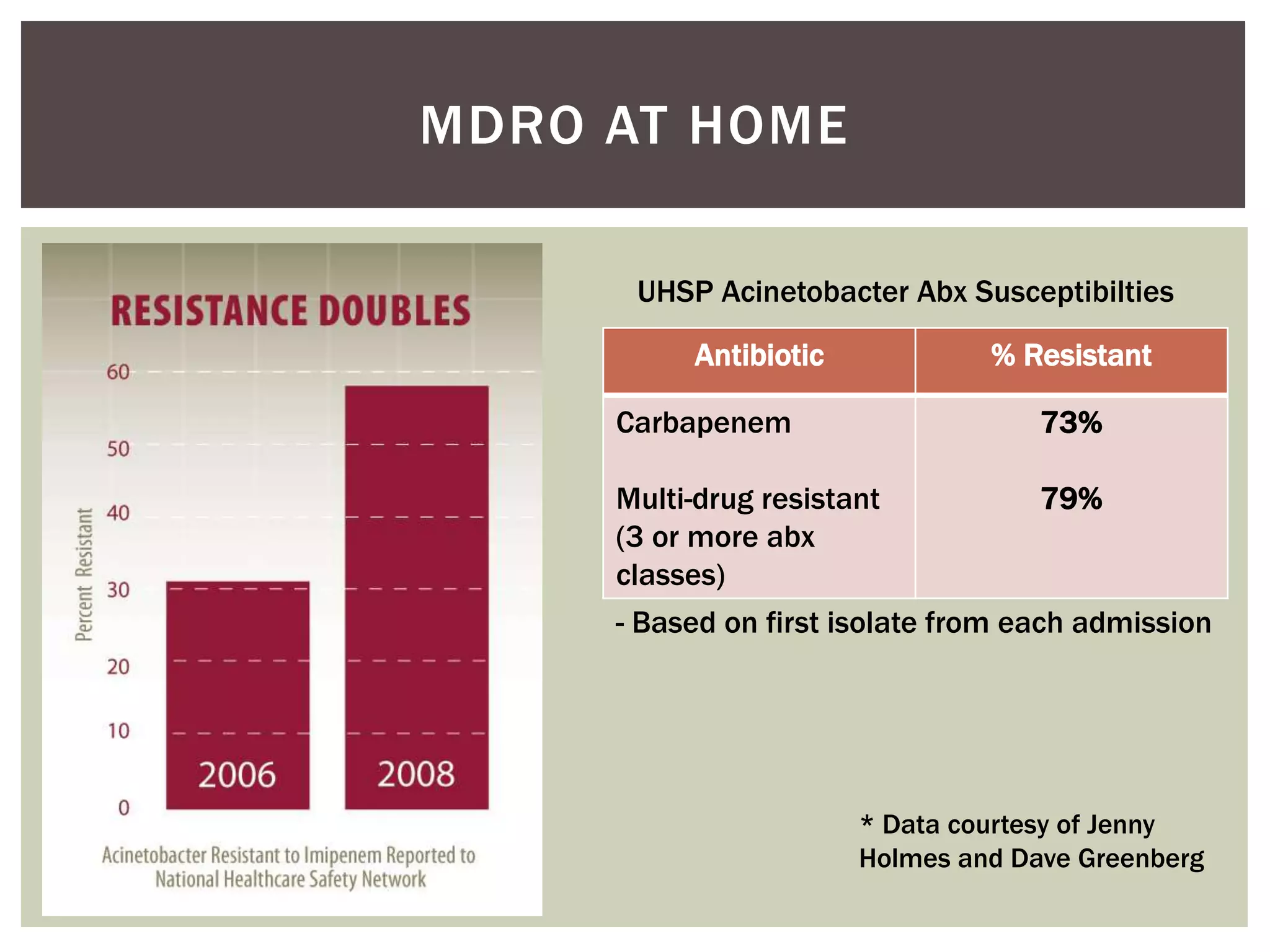
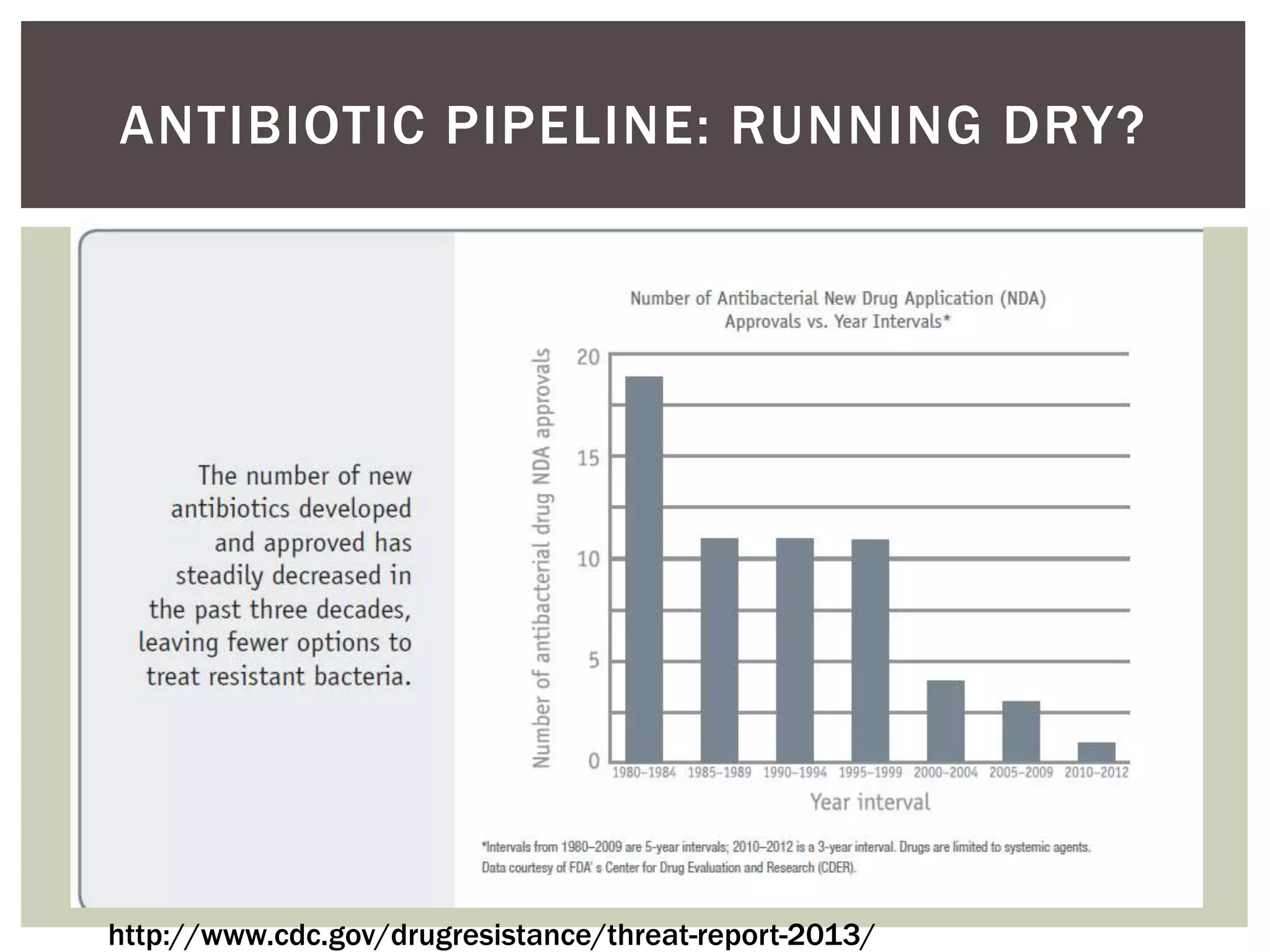
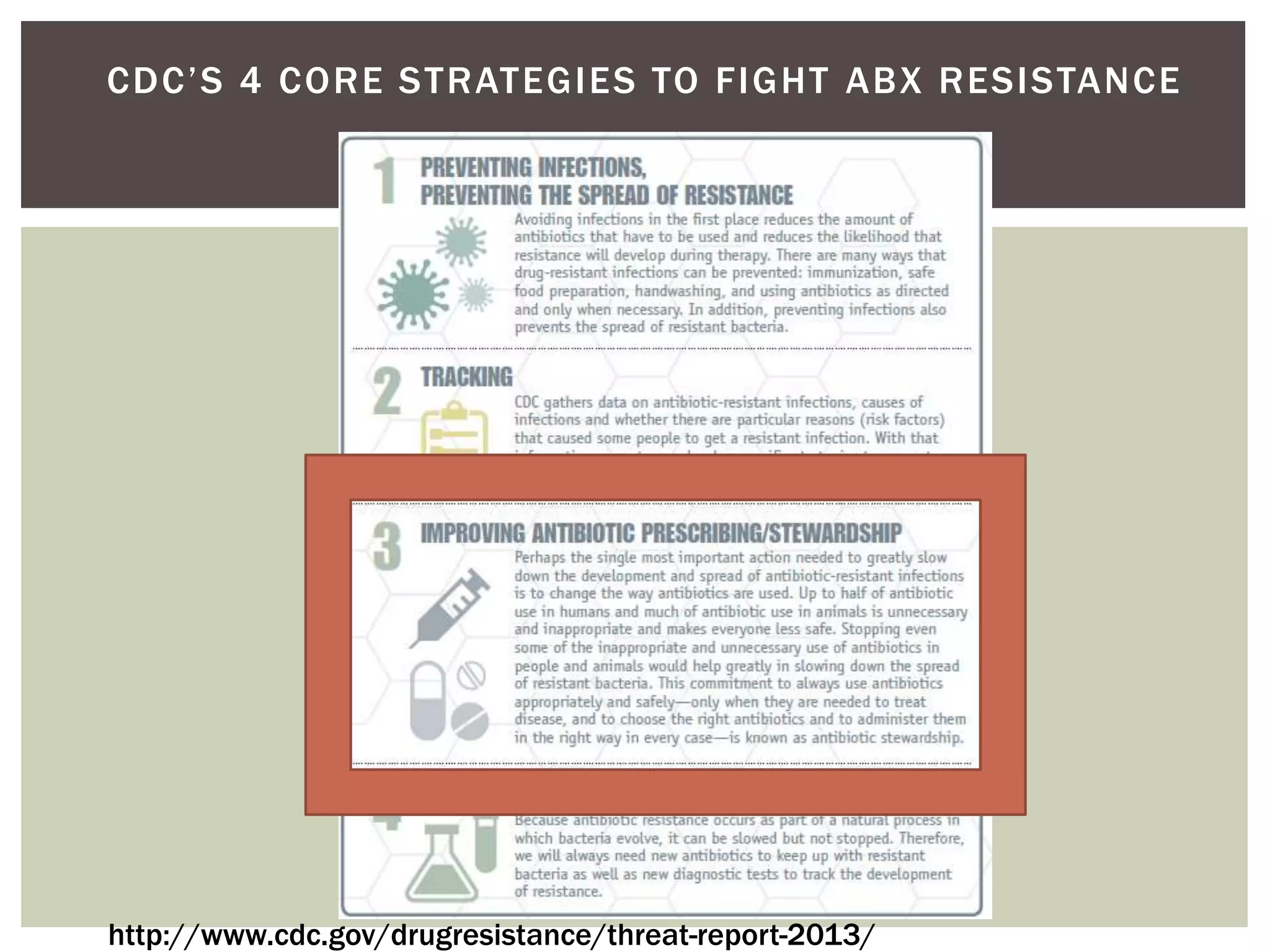
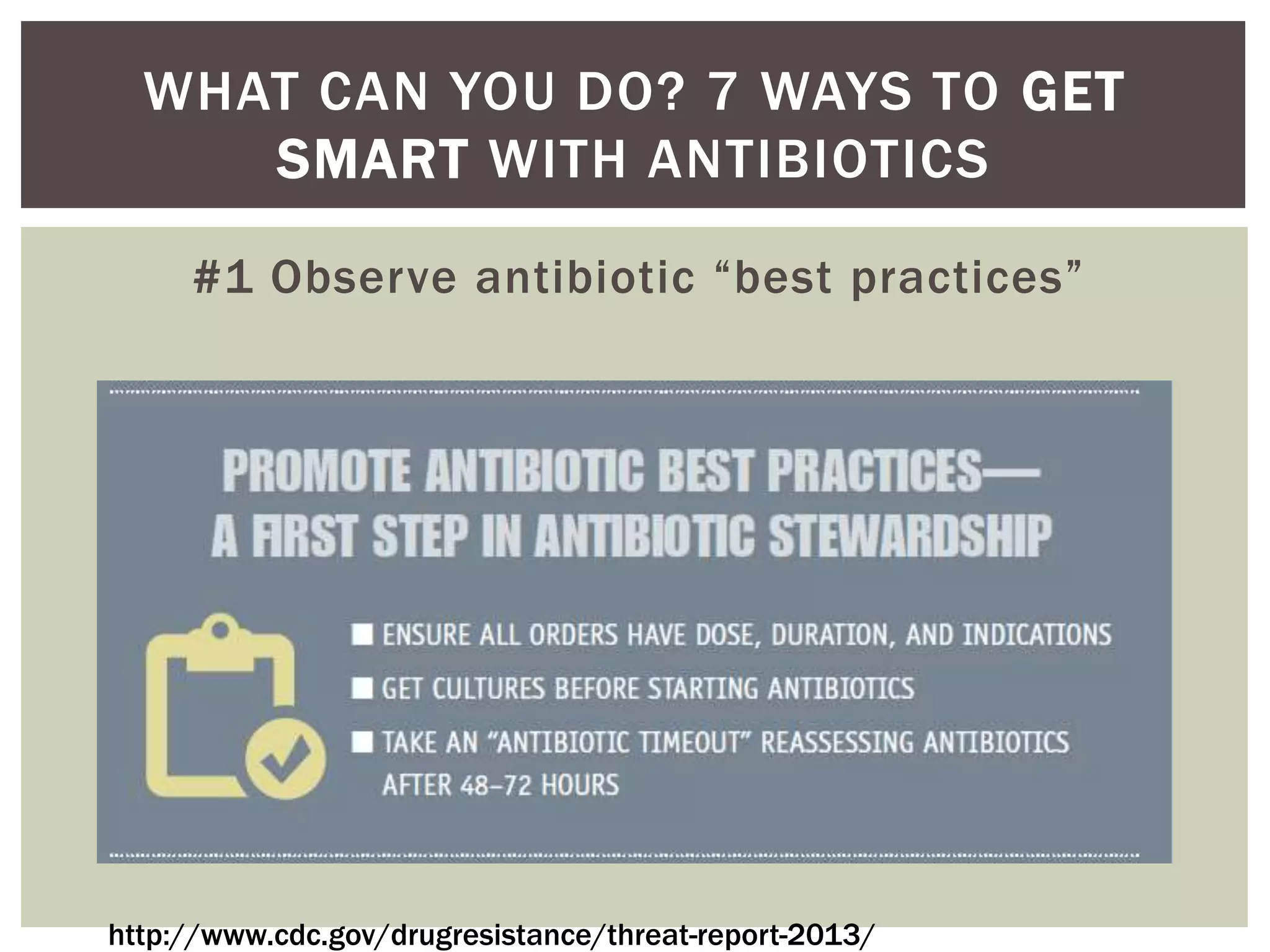
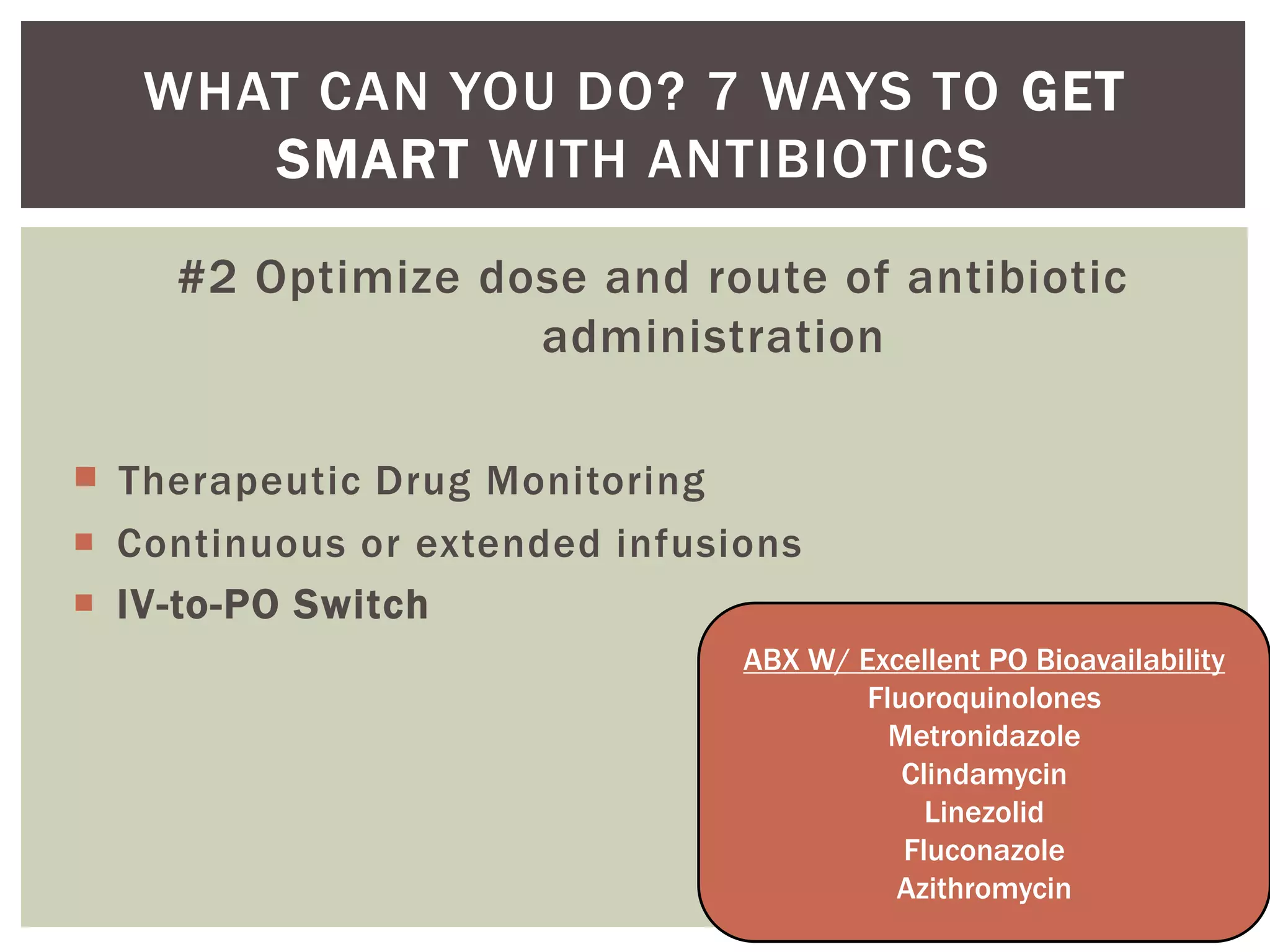
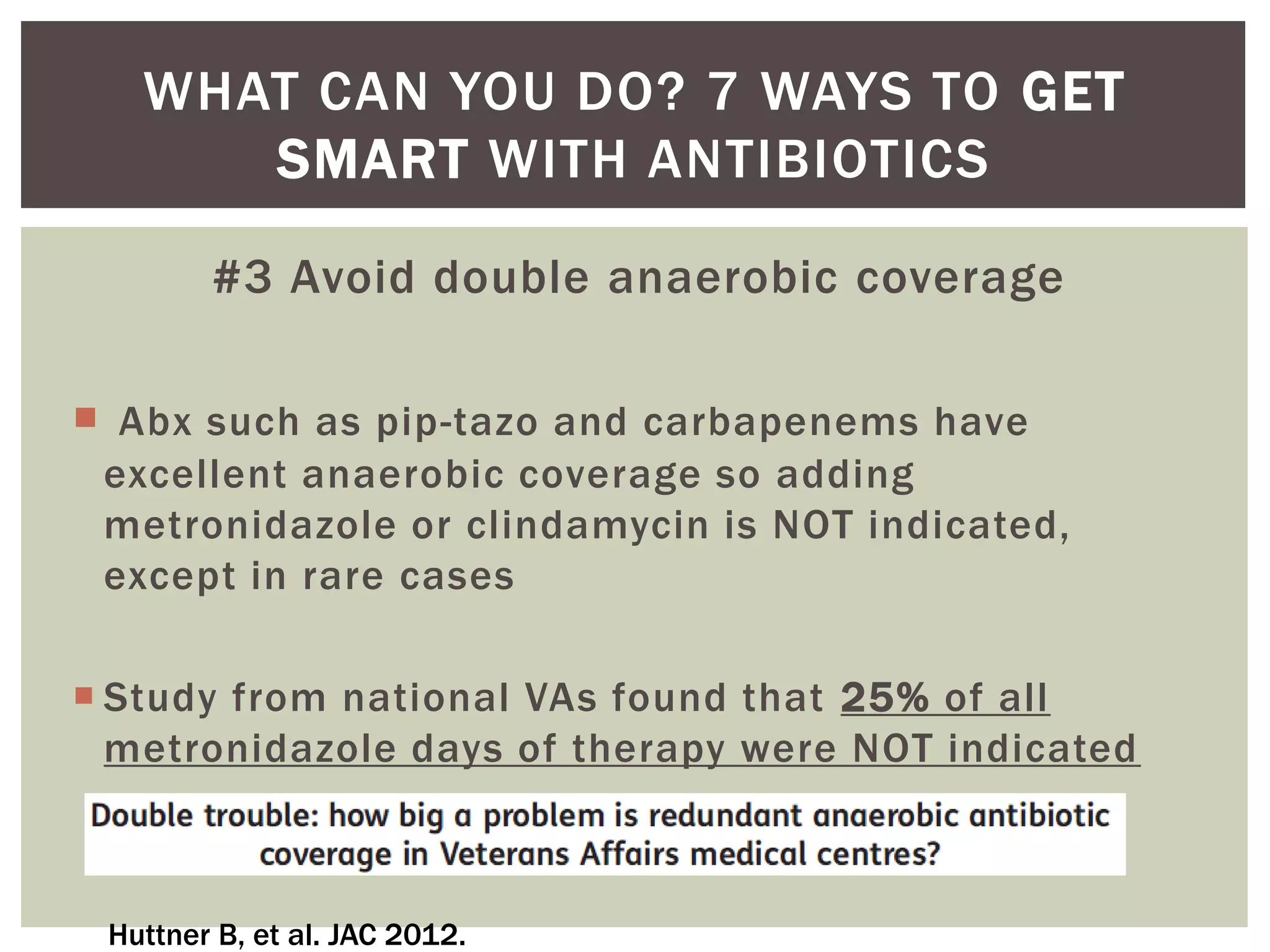
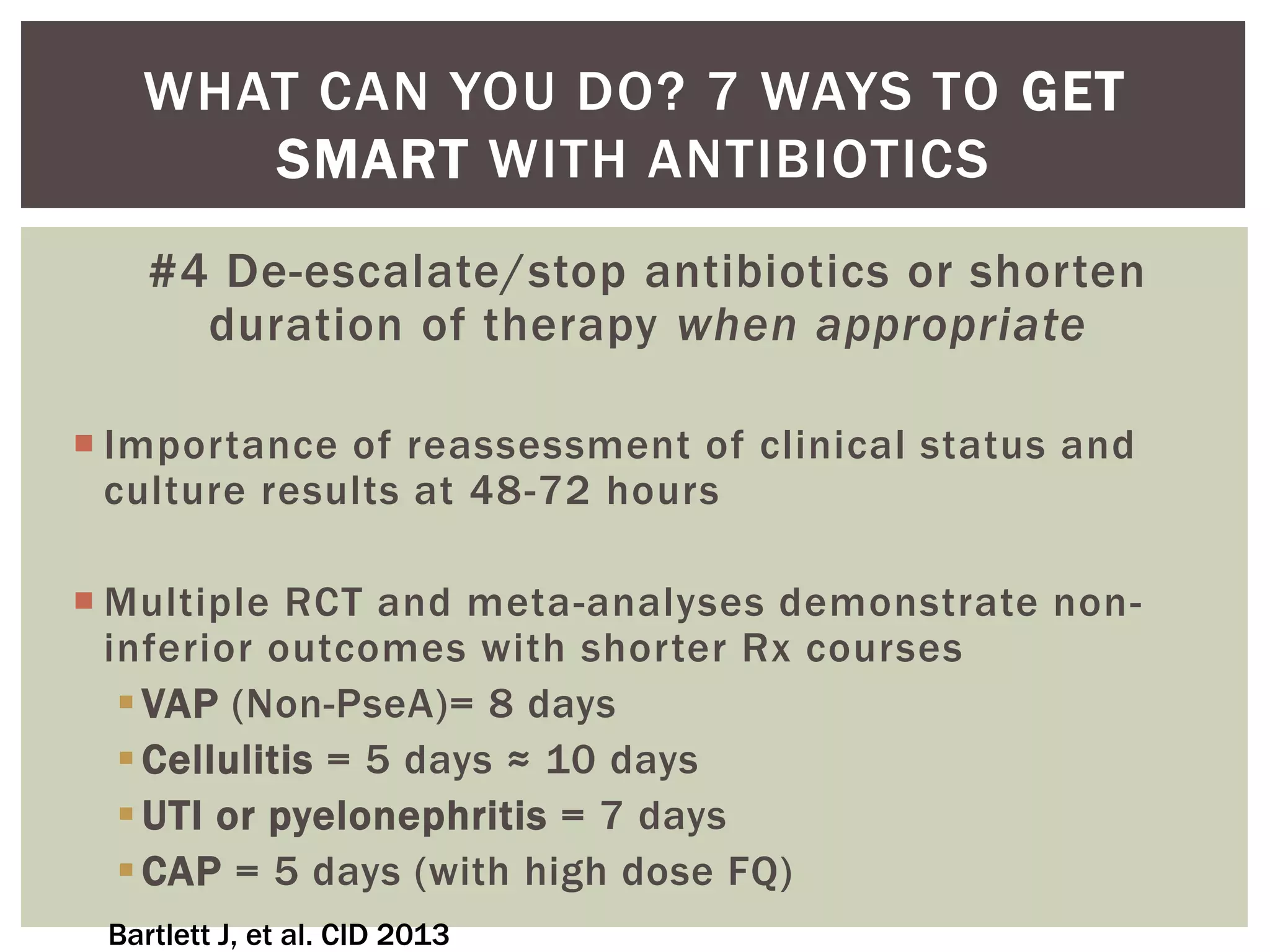
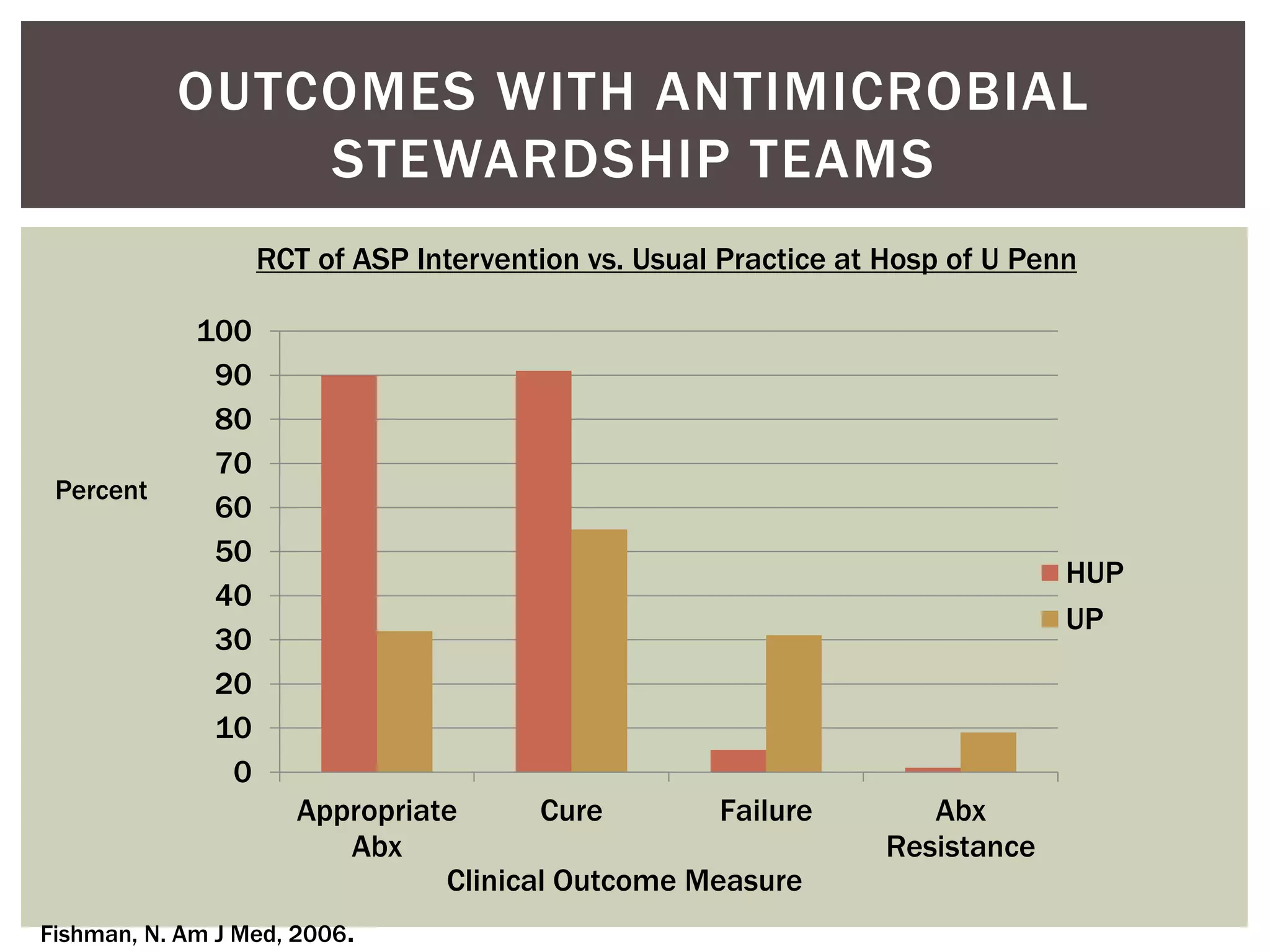
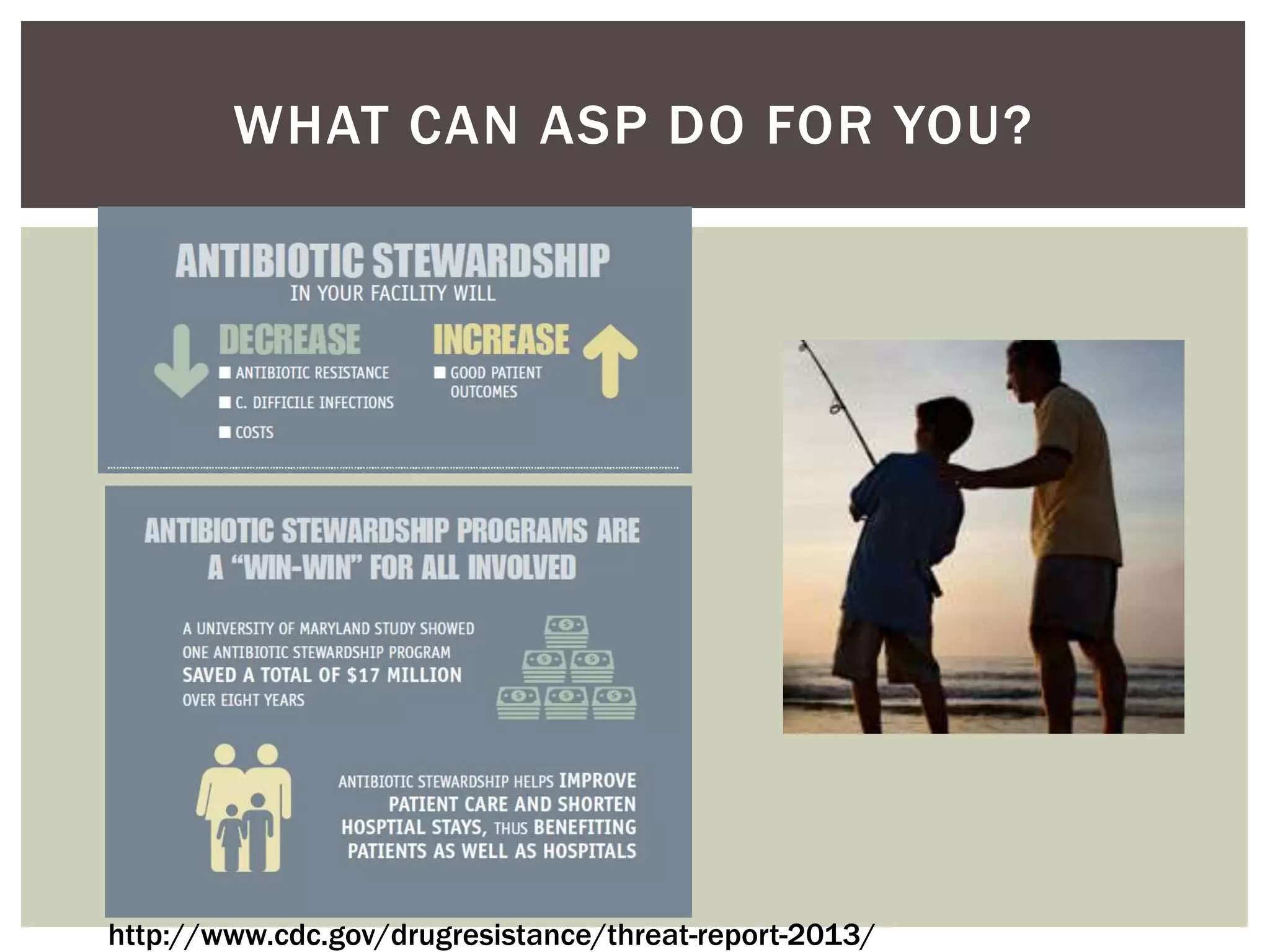
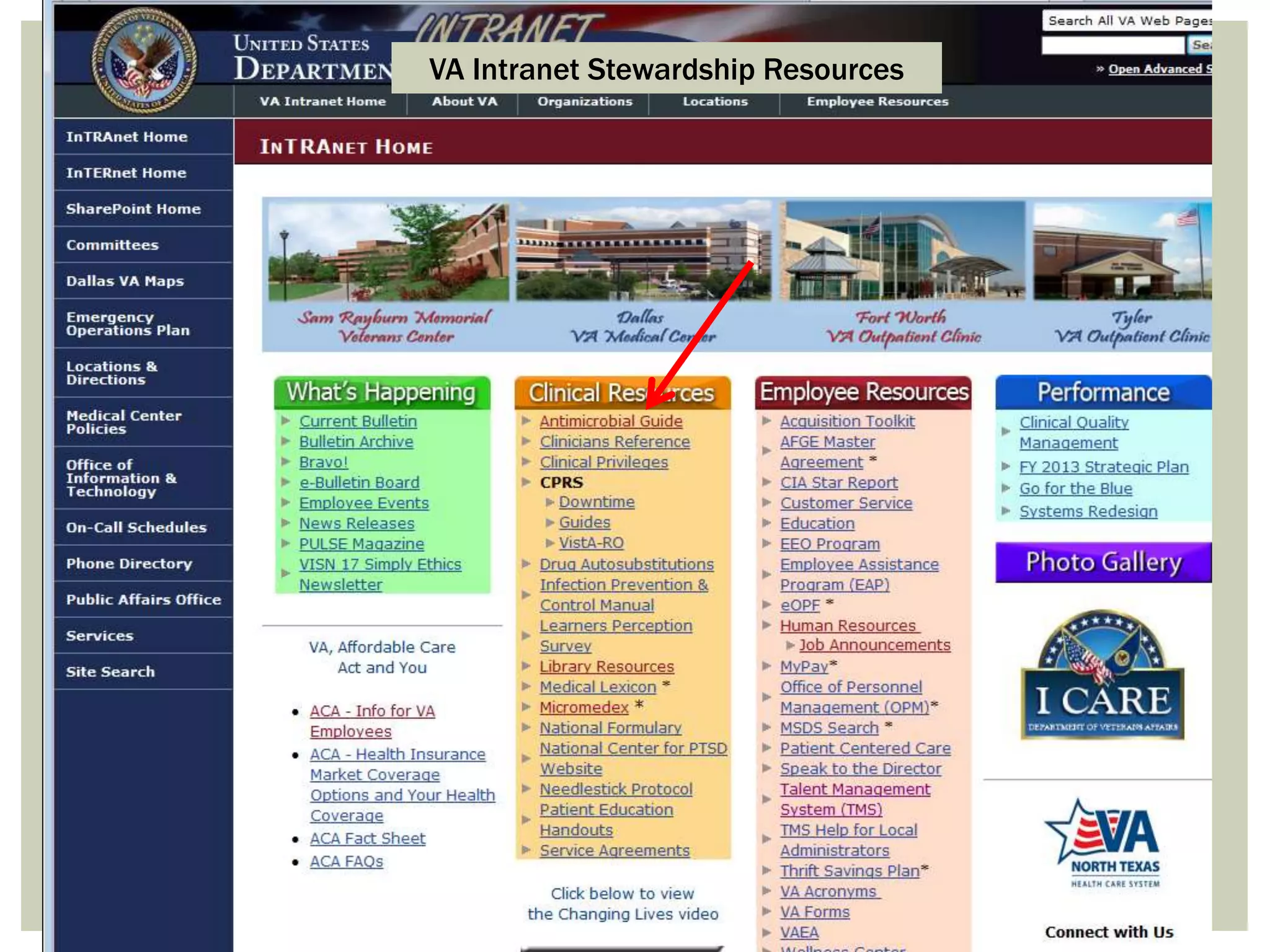
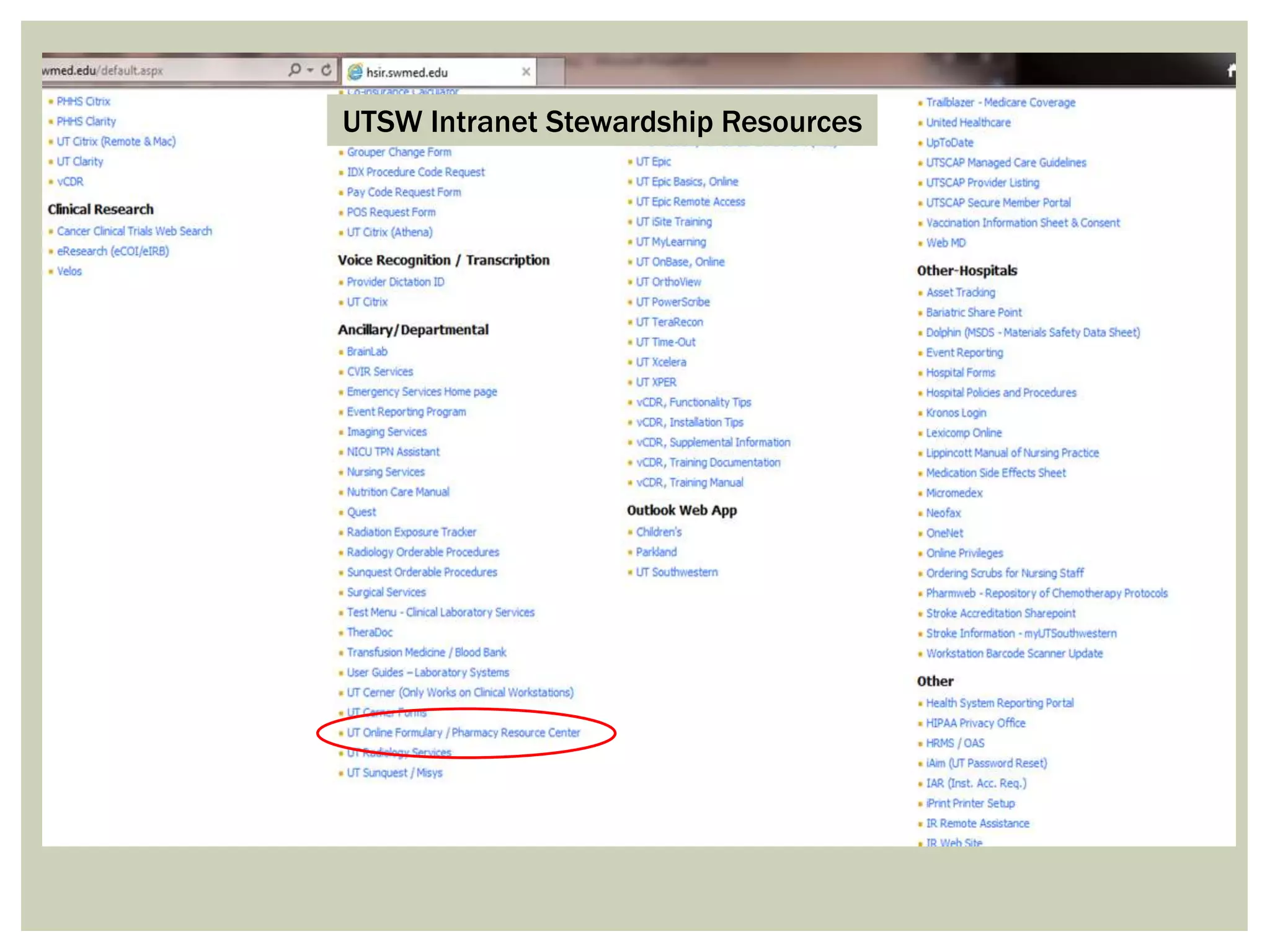
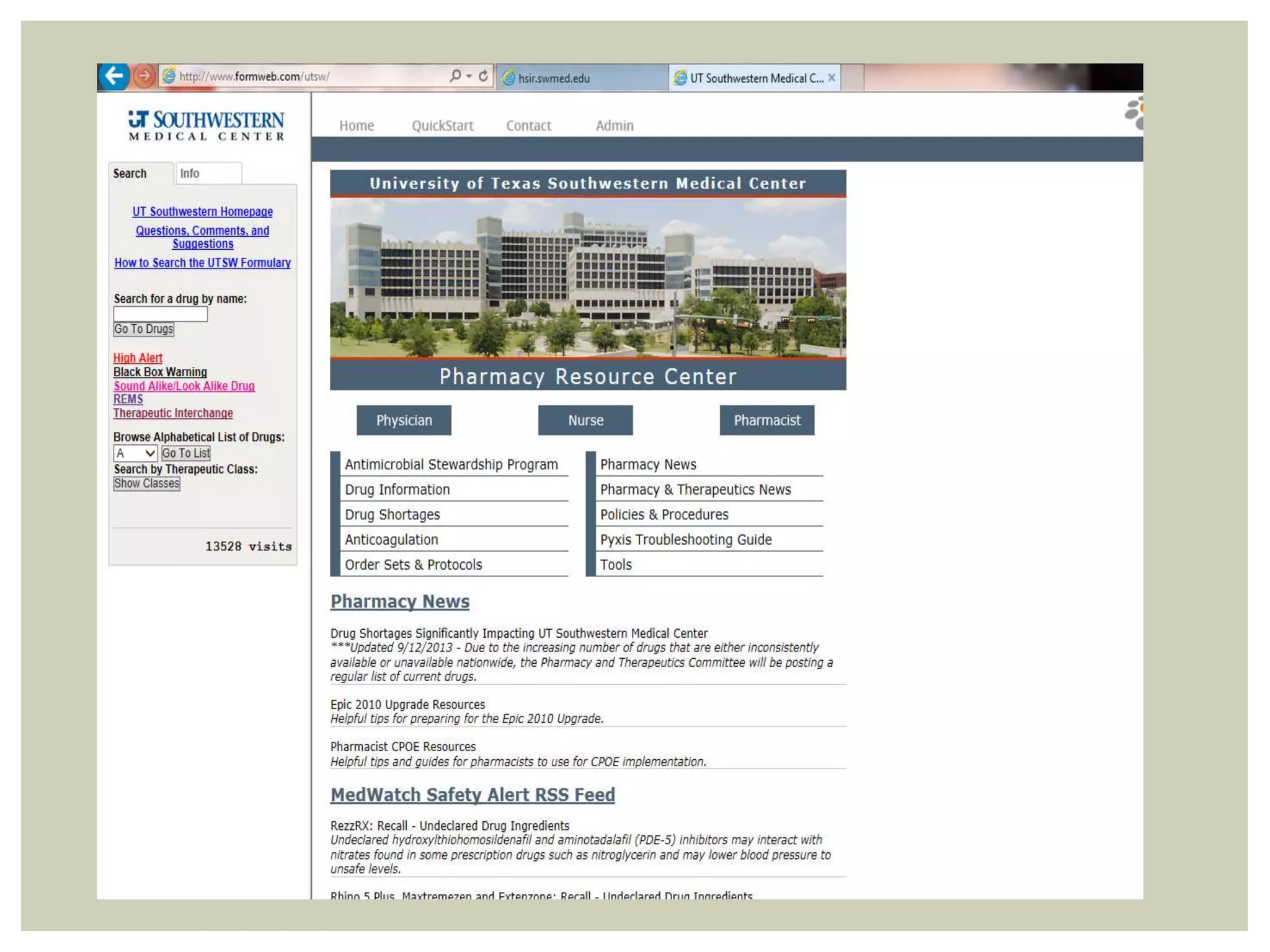
This document discusses antibiotic overuse and resistance. It notes that overuse of antibiotics can lead to adverse drug events, antibiotic resistance, and Clostridium difficile infections. It summarizes the 2013 CDC Threat Report on antibiotic resistance and lists several "superbugs" as major threats. The document advocates for antibiotic stewardship programs and lists seven ways healthcare providers can improve antibiotic prescribing practices to help address the growing crisis of antibiotic resistance.